
How ISQ guides clinical decisions – Insights from Dr. Paolo Carosi and Dr. Claudia Lorenzi
Sep 19, 2025
At Osstell, we believe in sharing real-world experiences from clinicians around the globe. This case study from Dr. Paolo Carosi and Dr. Claudia Lorenzi, two experienced implantologists and prosthodontists from Italy, offers valuable insights into how ISQ measurements support treatment decisions. With the full study now published in the International Journal of Oral Implantology, we are pleased to highlight some of the most valuable findings for our community.

Dr. Paolo Carosi and Dr. Claudia Lorenzi.
Our starting point
The use of dental implants for oral rehabilitation has become a well-established procedure for predictability and patient satisfaction. This success is the result of decades of extensive research into the biology of implant wound healing, osseointegration, and tissue remodeling. Modern implantology bases its success on osseointegration, specifically on the transition from mechanical retention to biochemical bonding of newly formed bone to the implant surface. In-depth knowledge of the molecular and biological events responsible for osseointegration has led to exponential advancements in dental implantology, including the commercialization of improved macrodesigns, implant roughness, and hydrophilic surfaces. However, clinical evaluation of the dynamics of implant wound healing, their interpretation, and their application to personalized protocols are still lacking and represents an opportunity for improvement in the field.
What’s still missing in the literature?
Although osseointegration is fundamental in dental implantology, there is limited availability of tools for quantitatively evaluating osseointegration and its progression in clinical settings. The usage and interpretation of those tools are often under-reported in the literature, resulting in standardized clinical protocols that lack customization based on individual patient profiles. Current literature lacks systematic ISQ assessment for long-term follow-ups, often, there are no intermediate measurements reported to track changes between initial and final evaluations.
Why and how?
This study aimed to assess longitudinal changes in ISQ values over one year, measured monthly, to better understand dynamics of wound healing and the development of implant stability for hydrophilic self-tapping tissue level implants and to further validate RFA technology and its application in clinical practice.
31 patients (19 females and 12 males; mean age 53.81 ± 9.48 years) were treated and monitored monthly over the course of one year following implant placement. A total of 50 dental implants (mandible: 25, maxilla: 25; immediate: 15, delayed: 35) were installed without protocol deviations and remained free from biological or mechanical complications throughout the 12-month observation period (implant survival rate: 100 per cent; prosthetic success rate: 100 per cent). ISQ was recorded at the time of placement (t0) and at each monthly follow-up (t1 to t12).
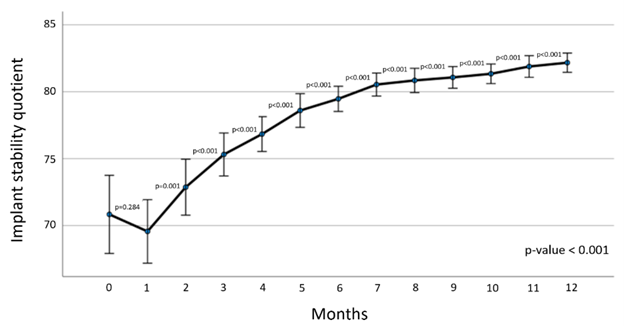
ISQ at each timepoint resulted significantly greater than the previous timepoint (p-value < 0.001; t2-t1, t3-t2, t4-t3, … t12-t11), except for the pair t1-t0, where negative but non-statistically significative values were observed (p-value = 0.28). From t3 onwards, every measurement is statistically significantly greater than at t0 (p-value < 0.0001; t3-t0, t4-t0, t5-t0, … t12-t0). In terms of the temporal dynamics of implant stability, stability decreased until it was lowest at 1 month after implant placement, then consistently increased every month for 1 year without plateauing. (Figure)
Results that confirm the current literature
Classical studies have reported an initial phase of bone remodeling where old bone used for primary mechanical retention is resorbed, and new bone is formed in contact with the implant surface. This initial phase can lead to a temporary reduction in stability, with the overall lowest value at one month after implant placement. On average, implant stability was significantly greater from the third month onward compared to the time of implant placement. A translational interpretation of this clinical finding is that only at the third month secondary stability surpasses in strength the mechanical retention that existed at time of implant placement.
Something new in immediate implants
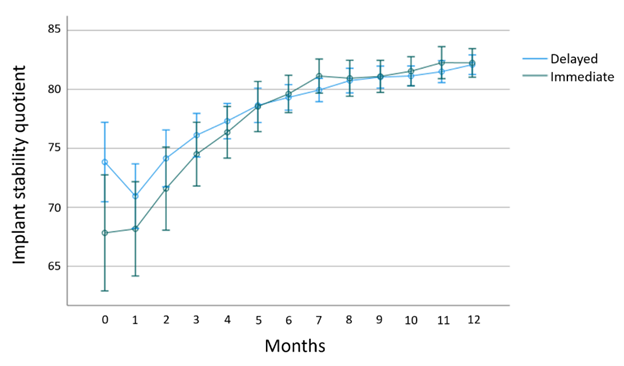
An interesting clinical comparison was between delayed and immediate implants. Delayed implants achieved higher ISQ at the time of placement compared to immediate implants, possibly due to the lower volume of native bone engaging the immediate implants. However, immediate implants exhibited a more rapid increase in stability until no difference was found between the two groups. This supports the idea that molecular processes toward secondary stability follow a similar path regardless of whether the implant placement is immediate or delayed. While the remodeling process eventually eliminates the initial advantage of the higher mechanical stability of the delayed implants. (Figure)
What we learned after one year
After many ISQ measurements during this long follow-up, we started to anticipate the ISQ values and to understand why each clinical scenario would result differently from one another.
A deeper understanding of RFA as a clinical measure of subclinical wound healing events could lead to significant advancements in both research and clinical practice. Based on our findings, we can conclude that:
- Overall implant stability decreases to its lowest values 1 month after implant placement, followed by a consistent increase without reaching a plateau within the study period. A high ISQ at placement predicted a larger ISQ drop at 1 month.
- Immediate implants had lower initial ISQ, but were followed by a steep increase, whereas delayed implants had higher initial ISQ values but were followed by a flatter increase, resulting in no final differences between the timing protocols.
- ISQ value measurement is a safe and non-invasive diagnostic tool of implant stability that showed fluctuations as a measure of wound healing events.
- Future research will emphasize and test similar clinical scenario with similar implants, trying to decode biological changes into numbers.
Read the full study
Published in the International Journal of Oral Implantology, the full case study by Dr. Paolo Carosi and Dr. Claudia Lorenzi is available here 1.
Learn More About ISQ and Osstell Technology
- The Osstell ISQ scale – Understand how ISQ values are interpreted and used in clinical decision-making. Read more here.
- The technique behind Osstell – Dive into the Resonance Frequency Analysis (RFA) method and how it works. Read more here.
About the Authors
Dr. Paolo Carosi, DDS, PhD graduated from the University of Rome Tor Vergata in 2017, where he also completed a Master in Digital Dentistry (2018) and earned his PhD (2022). Dr. Carosi has lectured on digital implant technologies at various prestigious universities including the University of Michigan (USA), University of Rome “La Sapienza” (Italy), and University of Pune (India). He is an active ITI member, serving as ITI Study Club Director and in the Young ITI Italian Committee. He runs his private practice and research in the clinic “CL Dentistry” (Segni, Italy) together with Dr. Claudia Lorenzi.
Dr. Claudia Lorenzi, DDS, PhD graduated from the University of Rome Tor Vergata in 2016, where she also earned her PhD (2019) researching dynamic navigation systems accuracy and completed her Oral Surgery residency (2025). Her research focuses on digital technologies for implant surgery and prosthodontics, for which she has received numerous national and international awards. She runs his private practice and research in the clinic “CL Dentistry” (Segni, Italy).
Reference
*Carosi P, Lorenzi C, Di Gianfilippo R, Campanella V, Wang HL, Arcuri C. Effect of time and local factors on the stability of hydrophilic self-tapping tissue-level implants: 1-year prospective study. Int J Oral Implantol (Berl). 2025 Sep 8;18(3):225-240.
https://pubmed.ncbi.nlm.nih.gov/37301374/



Add comment