20 years of Resonance Frequency Analysis in implant dentistry – a milestone review
Aug 28, 2025
In this article, we revisit the 2013 review by Prof. Lars Sennerby, which summarizes two decades of clinical and scientific experience with Resonance Frequency Analysis (RFA) — the method behind the Osstell technique.
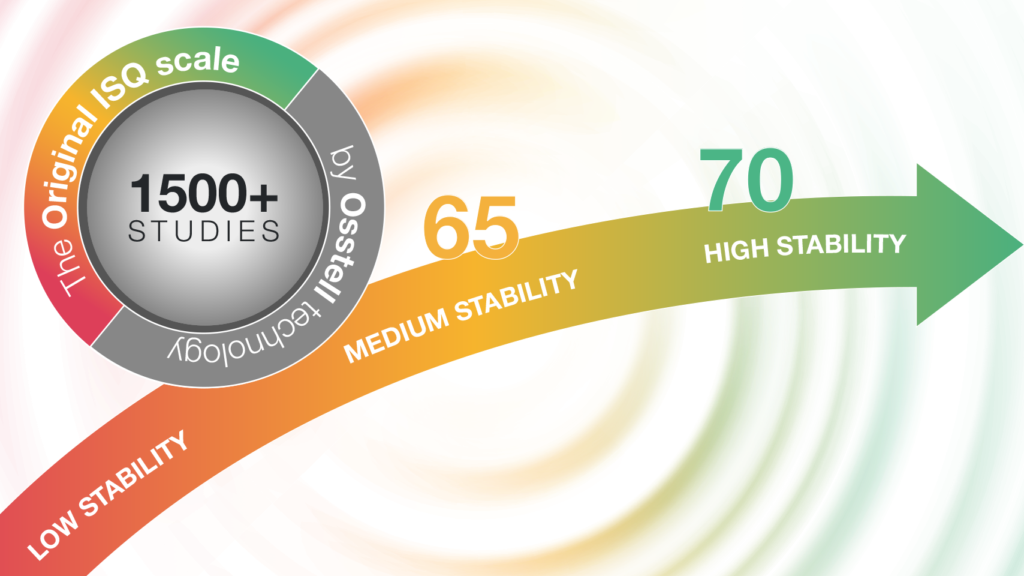
This publication, titled “20 Jahre Erfahrung mit der Resonanzfrequenzanalyse”, is available in German only and represents the first of nine key studies that form the scientific foundation for the recommendations in our current ISQ scale. While more than 1,500 studies support and validate the use of ISQ measurements, these nine have been selected for their strong clinical relevance and clear validation of the scale and its thresholds.
Read the abstract and access the full review.
Understanding ISQ – the Implant Stability Quotient
At the heart of the Osstell technique lies the ISQ scale, ranging from 1 (lowest stability) to 99 (highest stability). ISQ values are derived from RFA measurements and reflect the stiffness of the bone-implant interface. These values are influenced by several factors, including:
- Bone density
- Surgical technique
- Implant design
- Healing time
- Exposed implant height
Why ISQ matters
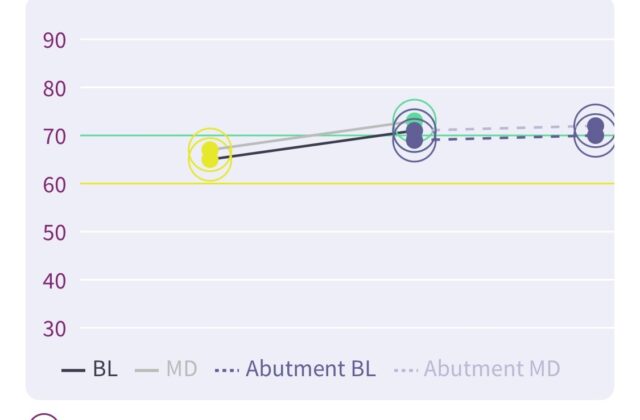
Prof. Sennerby’s 2013 review underscores a critical insight: implants with low or decreasing ISQ values are at a higher risk of failure compared to those with high or increasing values. This correlation has been consistently observed across both animal models and clinical studies.
ISQ measurements provide clinicians with objective feedback starting at the time of surgery and throughout follow-up, supporting more informed decisions regarding:
- Surgical protocols
- Healing times
- Loading strategies
- Risk assessment and management
Clinical applications and decision-making
The Osstell technique has proven especially valuable in complex cases, such as immediate or early loading, grafted bone sites, and fresh extraction sockets. By monitoring ISQ over time, clinicians can detect early signs of instability and intervene before clinical failure occurs.
In his review, Sennerby proposed a framework for interpreting ISQ values. While the original thresholds have since evolved, the foundational concept remains central to clinical decision-making. Today, a more conservative version of the ISQ scale is commonly used:
- 🟥 Red zone (<60 ISQ): Extended healing or alternative strategies recommended
- 🟨 Yellow zone (60–69 ISQ): Monitor closely; consider delayed loading
- 🟩 Green zone (≥70 ISQ): Suitable for immediate loading
Note: This updated scale reflects current clinical experience and builds upon the principles outlined in Sennerby’s original work.
Conclusion
This 2013 review reaffirms the Osstell technique as a scientifically validated, clinically useful method for assessing implant stability. As implant dentistry continues to advance, tools like RFA will remain essential in ensuring predictable outcomes and long-term success.

Add comment