Treating osteoporotic patients
Jul 8, 2020
A review by Dr. Tara Aghaloo, D.D.S., M.D., PH.D.
Dr. Tara Aghaloo is Professor in Oral and Maxillofacial Surgery and Assistant Dean for Clinical Research at the UCLA School of Dentistry. She completed her dental training at the University of Missouri in Kansas City, and Oral and Maxillofacial Surgery residency and M.D. at UCLA. Subsequently, she completed a Ph.D. in oral biology at UCLA. She is a diplomate of the American Board of Oral and Maxillofacial Surgery (ABOMS), and a member of the ABOMS Examining Committee. Her clinical practice focuses on implant surgery and bone and soft tissue grafting, with a focus on treating medically compromised patients. She is also active in professional organizations where she is President-elect of the Academy of Osseointegration (AO), a fellow of both the AO and ITI, member of the ITI research committee, member of the AAOMS Research Committee, and section editor of IJOMI.
Please give us some background on the research you think is most important in this area of treating osteoporotic patients and managing the effects of the drugs they take for the disease when considering dental implant therapy?
Dr. Tara Aghaloo: The research would support the importance of assessing not just the bone health of the patients but also assessing their overall health. In terms of bone health there should be an evaluation of the stage of the patient’s disease and whether it is osteoporosis or osteopenia. Knowing things about the patient such as family history of osteoporosis or osteopenia, bone related trauma, and history of fractures is also valuable information in treatment planning.
Obtaining the results of diagnostic tests such as bone density scans as well as information on any treatments the patient is having or has had would also be important. Some treatments may be non-medical therapy such as weight bearing exercise, special dietary plans and the use of supplements. The complete history of medications, both current and previous, should be considered as some osteoporosis medications have effects that remain for more than 10 years
- Previous dental history and dental health (extractions, peri-apical or periodontal disease, implants, hygiene, maintenance regimen)
- Other medical conditions and medications (some conditions may exacerbate implant risk or alter bone health or healing capacity)
- Up to date research and guidelines on treating osteoporotic patients (see summaries and references below)
Please give us the highlights of the main results and conclusions that have come out of these studies. What implications do you think the results have for the dental implant treatment planning of these patients?
- Aghaloo T, Pi-Anfruns J, Moshaverinia A, Sim D, Grogan T, Hadaya D. The effects of systemic diseases and medications on implant osseointegration: a systematic review. IJOMI 2019;34(suppl):s35-49.
– 21 studies (4 studies had patients taking anti-resorptive medications and 17 studies had patients not taking them); these studies evaluated initial osseointegration, not necessarily long-term survival or success
– Although classically osteoporosis has been considered to associate with increased implant failure or poor stability, recent studies have not demonstrated a decrease in implant osseointegration. Caution, however, as osteoporotic patients are generally taking oral or parenteral anti-resorptive medications, and are at risk for osteonecrosis of the jaws (ONJ) - Stavropoulos A, Bertl K, Pietschmann P, Pandis N, Schiodt M, Klinge B. The effect of antiresorptive drugs on implant therapy: systematic review and meta-analysis. Clin Oral Impl Res 2018;29(suppl. 18):54-92.
– In 24 studies with oral bisphosphonate (BP) therapy and implants in patients with osteoporosis, no increase in implant failure, complications, or marginal bone loss was seen. However, cases of ONJ were seen in cancer patients receiving IV BPs (ONJ occurred sooner) or osteoporosis with long-term oral BPs (ONJ occurred later)
– Some studies with increased failure or marginal bone loss in osteoporotic patients not taking antiresorptives (Moy et al, 2005; Koszuta et al, 2015; de Souza et al, 2013)
– Caution with antiresorptive medications and implants, as many surgeries have identified implants as the inciting event, or ONJ occurring in the presence of previously placed implants - Jung RE, et al. ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin Oral Impl Res 2018;29(Suppl.16):69-77
– BP medications for osteoporosis were not associated with increased implant failure in the studies that were evaluated (1239 patients)
– No evaluation in cancer patients was performed
– Caution with the risk of ONJ - Schimmel M, Srinivasan M, McKenna G, Muller F. Effect of advanced age and/or systemic medical conditions on dental implant survival: a systematic review and meta-analysis. Clin Oral Impl Res 2018;29(Suppl.16): 311-30
– High implant survival in patients receiving low-dose antiresorptive medications for osteoporosis
– Caution with the risk of ONJ and other complications after implant surgery, especially in patients with cancer and taking antiresorptive medications; general contraindication for implants - Temmerman A, Rasmusson L, Kubler A, Thor A, Merheb J, Quirynen M. A prospective, controlled, multicenter study to evaluate the clinical outcome of implant treatment in women with osteoporosis/osteopenia: 5-year results. J Dental Res 2019;98(1):84-90
– Clinical trial with 5 year marginal bone loss measurements demonstrated no difference in maxillary implant survival or bone loss between healthy patients and those with osteoporosis or osteopenia
– Difficult to generalize to most osteoporosis patients, because the study did not include patients taking bisphosphonates (most osteoporosis patients are taking a bisphosphonate or other antiresorptive medication); also included both osteopenia or osteoporosis together - Lazarovici TS, Yahalom R, Taicher S, Schwartz-Arad D, Peleg O, Yarom N. Bisphosphonate-related osteonecrosis of the jaw associated with dental implants. J Oral Maxillofac Surg 2010;68:790-6
– Study of 27 patients (chart review from 2003-2009) with bisphosphonate-related ONJ associated with dental implants; 11 (41%) developed ONJ from oral bisphosphonates (BPs) and 16 (59%) from intravenous BPs
– The timing in this study was critical, as some ONJ occurred directly from the implant surgery, whereas some occurred many months or years after the implants were placed; there were even a few cases when the implants were already present before BPs were started. - Overall clinical implications
In general, implants in patients with osteoporosis are safe and effective; they seem to osseointegrate well, and can be maintained over the long-term. However, some studies have identified osteoporosis as a risk factor for implant failure. A very detailed history of medications (especially antiresorptives), dosing, and length of use must be evaluated and patients must understand a potential risk for osteonecrosis of the jaws (ONJ). A discussion of these issues must be included in the informed consent process with these patients.
My personal recommendations are to proceed slowly with implants in these patients, especially when the osteoporosis is severe, or extensive use of antiresorptive medications have occurred. If extraction sites have healed well, then implants will most likely heal well too. We don’t have to immediately load everything, or immediately place implants in these patients.
What do you conclude about the value of Osstell ISQ measurements in treatment planning these patients?
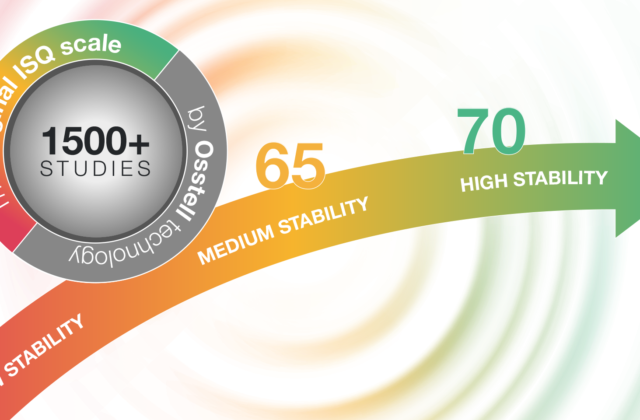
Dr. Tara Aghaloo: Since the posterior maxilla has been shown to have decreased implant survival due to poorer quality and quantity of bone (Moy et al., 2005) utilizing Osstell ISQ measurements can assist in following the osseointegration process, especially comparing Osstell ISQ at placement, stage 2 procedure, and crown delivery.
The transition from primary (mechanical) to secondary (biologic) stability is the most important aspect of implant treatment in osteoporosis patients, especially those taking antiresorptive medications. This is because remodeling needs to occur for osseointegration to take place, and the Osstell ISQ measurements can capture that osseointegration and give the clinician confidence that the implant is stable and ready to restore.
Any other comments or suggestions for your colleagues reading this?
Dr. Tara Aghaloo: We must be very diligent in our informed consent process, especially as our patients continue to become more medically compromised and take more medications that can alter the healing process. These are inherent risks of surgery, especially elective surgery. We must also continue to utilize objective measurements to evaluate healing and specifically osseointegration. Osstell ISQ values are one of the only tools that provide an objective measurement.
Thank you Dr. Tara Aghaloo for an insightful review!