
Yellow – Caution! Why ISQ 60–69 requires careful evaluation
Sep 08, 2025
This is the second post in our three-part series on the Osstell ISQ scale. After exploring the red zone, we now turn to the yellow zone — a transitional area where implant stability is improving but still requires careful monitoring. Understanding this zone helps you make informed decisions about loading protocols and healing strategies.
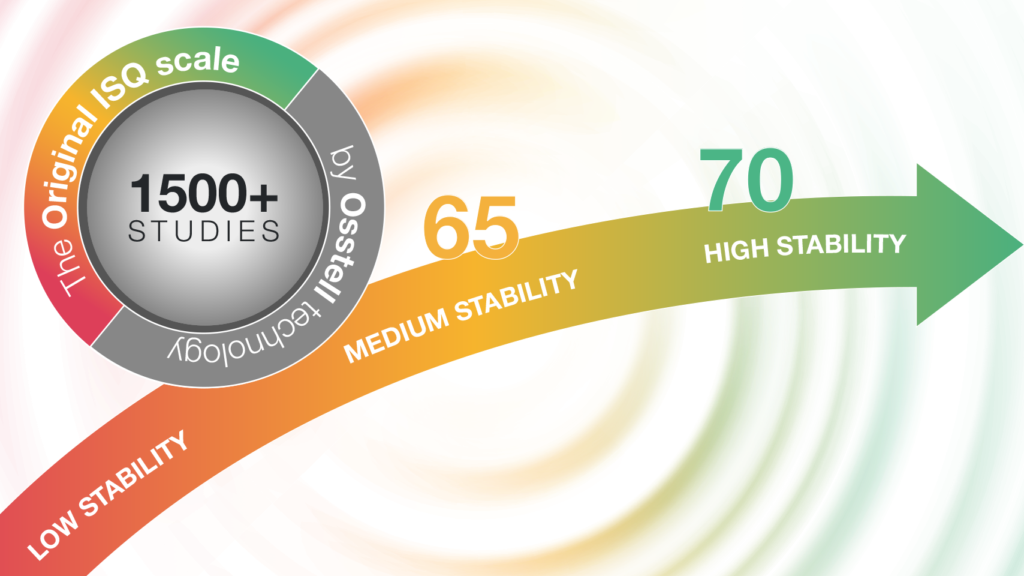
In implant dentistry, not all cases are clearly stable or unstable. The yellow zone on the Osstell ISQ scale — ISQ 60 to 69 — represents a transitional range where clinical judgement becomes essential. While the numerical difference between ISQ 60 and 70 may seem small, the biological difference is not: a 10-point increase in ISQ corresponds to approximately 50% greater implant stability, as demonstrated in a finite element analysis conducted by Semcon. Ref 1.
That’s why this zone deserves special attention.
This article focuses on how clinicians can navigate the yellow zone with confidence. Based on current evidence, we outline how to interpret ISQ values in this range, when to proceed, and when to wait. We also highlight how ISQ guidance can bring clarity and peace of mind in clinical decision-making.
Yellow – Caution!
The yellow zone on the Osstell ISQ scale — ISQ 60–69 — means proceed with caution. It’s not a warning sign, but a reminder to evaluate the full clinical picture. In this article, we explore how to act when encountering a yellow measurement at the time of implant placement or during follow-up. With the right tools and protocols, clinicians can make informed decisions and feel confident in their treatment plans.
The power of measurement: Confidence through clarity
The Osstell Beacon’s traffic light system — red, yellow, green — translates complex stability data into intuitive guidance. In the yellow zone, this guidance becomes especially valuable. It helps clinicians pause, reflect, and make decisions based on objective data rather than assumptions.
Don’t guess. Measure.
ISQ values in the yellow zone might not be a reason to worry — but they are a reason to pay attention.
What the evidence tells us about ISQ 60–69
1. A zone of transition and variability
Bornstein et al. (2009) provide valuable insight into the clinical relevance of ISQ values in the 60–69 range. In their prospective study, titanium implants with a chemically modified SLA surface were placed in the posterior mandible and loaded after just 3 weeks of healing. While initial ISQ values varied, the implants demonstrated a consistent increase in stability over time — from a mean ISQ of 74.33 at placement to 83.82 at 6 months. Importantly, even implants that initially showed borderline stability (including two “spinners” at day 21) achieved successful integration when managed appropriately. These findings underscore that ISQ values in the yellow zone can still lead to predictable outcomes, provided that clinicians monitor trends over time and consider the full clinical context, including bone quality and surgical technique. Ref 2
2. Immediate loading in splinted situations — with the right conditions
When implants are rigidly or semi-rigidly splinted, immediate loading can be safely carried out even at moderate ISQ values. A clinical study demonstrated that ISQ values remained stable between 45 and 75 over an 8-month period, with no significant difference between rigid and semi-rigid splinting. This suggests that splinting helps maintain implant stability and supports immediate loading protocols within the yellow ISQ zone (60–69). Ref 3
3. Micromovements still a risk
A retrospective study by Trindade et al. (2019) showed that implants with ISQ values in the 60–69 range can be successfully immediately loaded if splinted in full-arch cases, where mechanical stability is reinforced by rigid cross-arch splinting. However, the study also highlights that isolated or partially splinted implants in this ISQ range are more vulnerable to micromovements that can disturb healing. These findings support a more cautious approach in partial or single-unit cases, where one-stage surgery with early or conventional loading may be preferable. Re-measuring ISQ at 6–8 weeks (or earlier) is recommended to ensure sufficient biological stability before functional loading. Ref 4
Evidence-based recommendations for ISQ 60–69
At the time of surgery:
- Evaluate the full clinical context — bone quality, insertion torque, and ISQ.
- Consider a two-stage approach if ISQ is in the lower 60s or if risk factors are present.
- If proceeding with one-stage surgery, plan for delayed or conventional loading.
- Re-measure ISQ before final restoration to confirm biological stability
During follow-up:
- Monitor ISQ trends — an increasing value supports progression, while a decreasing or stagnant value may require intervention.
- Use OsstellConnect to visualise and document stability development.
- Let ISQ guide your timing — not the calendar.
Helping clinicians feel confident
The yellow zone can feel uncertain — but it doesn’t have to. With ISQ as a guide, clinicians can make informed decisions and feel confident in their expertise. OsstellConnect supports this process by providing a clear overview of each implant’s stability journey, helping clinicians stay in control and communicate clearly with patients.
Summary
Red – Stop!
Yellow – Caution!
Green – Go!
The yellow zone is not necessarily a warning — it’s a window of opportunity. It’s in this range that ISQ measurement becomes especially valuable. Knowing that an implant falls within the yellow zone allows clinicians to make informed, proactive decisions — such as choosing a two-stage surgical protocol or extending the healing period — that can have a decisive impact on treatment success.
By using ISQ as a guide, clinicians can tailor their approach to each patient’s unique situation, reduce uncertainty, and increase the likelihood of a predictable outcome.
Don’t guess. Measure.
References
1: Semcon. Finite Element Analysis of Osstell ISQ and Micro Mobility. Commissioned by Osstell AB. February 11, 2013. (Unpublished internal report)
2: Bornstein et. al. Early loading of nonsubmerged titanium implants with a chemically modified sand-blasted and acid-etched surface: 6-month results of a prospective case series study in the posterior mandible focusing on peri-implant crestal bone changes and implant stability quotient (ISQ) values, Clin Implant Dent Relat Res. 2009
3: Lee et. al. Implant Stability Measurements of Two Immediate Loading Protocols for the Edentulous Mandible. Rigid and Semi-rigid Splinting of the Implants, Implant Dentistry, 2012
4: Bavetta et. al. A Retrospective Study on Insertion Torque and Implant Stability Quotient (ISQ) as Stability Parameters for Immediate Loading of Implants in Fresh Extraction Sockets, BioMed Research International, 2019
Read more about and download the Osstell ISQ scale here.
You can find the other two blog posts in this series here:
Green – Go! Why ISQ > 70 means you can proceed with confidence – Osstell®
Red – Stop! Why ISQ < 60 means it is time to protect the implant – Osstell®



Add comment