
Primary and secondary stability is a much discussed topic. Which one should a clinician aim for to achieve successful implant treatments? We met with Dr. Stephen Jacobs after his lecture at the AO Annual Meeting about primary and secondary implant stability to clarify things.

Could you explain the difference between primary and secondary stability?
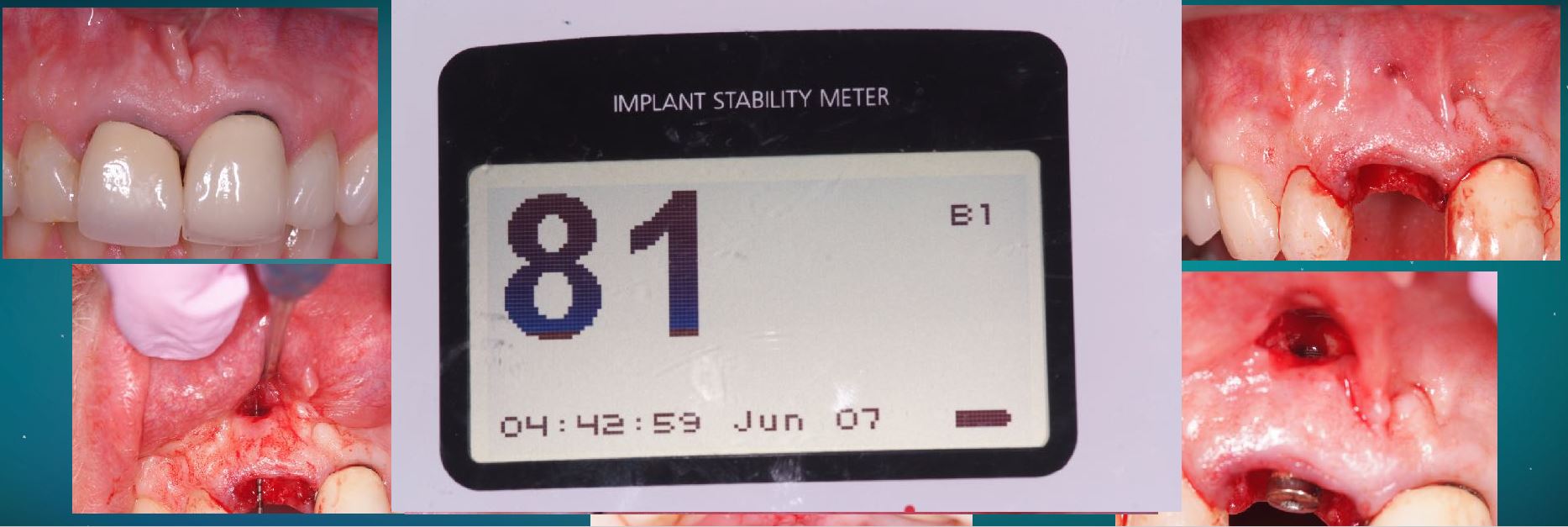
Dr. Stephen Jacobs: Primary stability is mechanical stability, the initial resistance to micro motion and micro mobility of a dental implant on insertion. It can be measured in a few ways, subjective evaluation, insertion torque, resonance frequency analysis or Periotest.
Secondary stability, on the other hand, is biologic stability or osseointegration. It is ultimately what determines the ability of the implant-retained restoration to withstand the functional forces, and become a functioning unit within a patient’s dentition.

You demonstrated that primary implant stability is not a key parameter, only secondary stability is of paramount importance for implant success. Why?
Dr. Stephen Jacobs: Primary, or initial, stability is important, as we do not want implants to be mobile within the osteotomy site. A degree of micro-movement is inevitable, but the issue is how do we measure it?
Most clinicians confuse primary stability with peak insertion torque, interchanging these terms, but insertion torque only measures one parameter, which is rotational resistance. Very simplistically put, our patients do nor load their implants to rotate, so I ask why do we get fixated (excuse the pun) on insertion torque?
More importantly, it is often described that to artificially increase this torque, we should undersize the osteotomy or utilise bone compression techniques. This has been shown clearly in the literature to have a detrimental effect on the healing process, potentially damage bone and delay the onset of osseointegration.
We should be interested in secondary stability, and achieving this as quickly as possible, at the same time allowing the periimplant bone to remain viable and stable, thus ensuring long term clinical success.

How does secondary stability improve treatment outcome?
Dr. Stephen Jacobs: Secondary stability is osseointegration, and as we know this is our ultimate goal. We ideally want to achieve sufficient secondary stability in a quicker time as possible so that our patients can return to normal function with their implant-supported restorations.
I believe that the maintenance of marginal periimplant bone is one of the key factors in preventing future biological complications, so if we can achieve secondary stability with minimal disruption to the bone at a cellular level, then we are going a long way to achieving long term predictable success.
With patients requesting shorter treatment times, how can measuring secondary stability can help clinicians meet this demand?
Dr. Stephen Jacobs: It is now accepted that resonance frequency, with a measurement of ISQ, allows clinicians to monitor the implants over time. The onset of osseointegration is a dynamic process where change takes place over time and RFA allows us to measure that change.
Of course, we like to measure insertion torque, it is one of our parameters at the surgical insertion of an implant, but it is a ‘one-time’ measurement, thus we cannot repeat it. An ISQ measurement records lateral stability or the resistance to micro-motion and micro-mobility, which of course represent the direction of forces applied to our implant restorations in function.
We can thus make an evaluation based on an objective measurement, on whether an implant can be immediately loaded or early loaded.
Thank you so much for your time Dr. Jacobs!
About Dr Stephen Jacobs, BDS: based in Glasgow (UK), he is passionate about dental implants and is a leading clinician in the field of implantology. He lectures throughout Europe on all aspects of dental implants, has published many articles and is on the editorial board of two journals. Stephen is a past President of the Association of Dental Implantology (UK). He was awarded Fellowship of the Academy of Osseointegration (AO).
More about implant stability:



Add comment