
At the Osstell ISQ Symposium 2021, we had the great honor of having Dr. William Martin as one of the speakers. Dr. Martin is a Clinical Professor in the department of Oral and Maxillofacial Surgery at the University of Florida’s College of Dentistry. He received his DMD with honors from the University of Florida and completed his MS and Certificate in Prosthodontics from Baylor College of Dentistry. Dr. Martin joined the faculty at the University of Florida in 1999 and serves as the Director of the Center for Implant Dentistry.
Questions and answers from the live Q&A
During Dr. William Martin’s lecture
“Utilizing Osstell ISQ to Streamline Patient Care and Improve Implant Education”, many questions came in from viewers. The most of them were answered by Dr. Martin during the Q&A session, but we have gathered them here in this blog post for you to enjoy during the days off in December.
Dr Martin, you mentioned that ISQ is a valuable tool in Immediate Cases. How do you apply the ISQ measurements taken in your determination to move forward?
Dr. William Martin: There are many clinical factors that are taken into consideration, and the ISQ is just one measurement that is utilized in the decision-making process. Other factors/measurements include:
a. Are we loading a single, segment/quadrant, or full-arch or implants? – this will influence the range of ISQ values that will trigger and immediate loading workflow.
b. Have we obtained primary stability with good apical bone support (>5mm)?
c. Was the insertion torque values greater that 25 Ncm?
d. Is the management of occlusion favorable in a patient with no parafunctional habits or compliance issues?
e. In single-tooth situations, where is the implant located – anterior, posterior?
Are 25 Ncm Insertion Torque and 60 ISQ equivalent values?
Dr. William Martin: No, they are complimentary, the insertion torque is influenced by the type and quality of bone present in the osteotomy site, the ISQ is influenced by the surface area contact between the bone and implant. At the time of surgery, they have their own influence on the decision to load the implant or not.
If you have a “spinner” implant, would you take it out, after healing place a new implant – or would you leave it in and use the Osstell for monitoring it, and expect it to gradually integrate?
Dr. William Martin: “Spinner” implants that have no vertical or oro-facial mobility and are associated with favorable peri-implant tissue health and radiographic evaluation are left to heal in an unloaded scenario. The ISQ measurement is a good data point to chart progress over time. We have successfully utilized this workflow in the past with these situations in our implant center.
Is finger tightening enough for the SmartPegs? I feel sometimes that I need re-tighten them and get a few units higher ISQ value.
Dr. William Martin: I like to utilize the air/water spray in the implant connection prior to placing the SmartPeg, and always attempt to achieve 5Ncm placement torque, which is sometimes hard to judge in clinical situations. As mentioned in the lecture, Osstell is working to develop a disposable placement device that will insure ideal tightening of the SmartPeg, in our clinical trials it has been met with favorable feedback.
Do you ever use ISQ Measurements to assess stability status of Implants in cases that you are treating due to complications and or potential redo?
Dr. William Martin: We like to get a baseline reading (when possible), on all implants we plan to restore in our practice. While not always achievable, when done it documents a stability starting point that we can build off from.
Can we use ISQ reading to predict prognosis of old ailing implant?
Dr. William Martin: I don’t believe a single measurement is the answer. When utilizing ISQ measurements in an ailing implant, you would like to want to see a reduction in values over time. Of important note – this is not independent of other diagnostic evaluations (i.e. radiographic, palpation, probing, etc…)
How does ISQ measurements on abutments differ from implant level readings? You mentioned it was not 1:1. Also are there specific SmartPegs for abutments?
Dr. William Martin: Yes, there are abutment specific SmartPegs, and the ISQ values are unique to that indication. i.e. implant level measurements and abutment level measurement on the same implant will not coincide.
How come you do not relate to the drop to Dr Paul Rosen‘s dip during the transition from primary to secondary stability? Great presentation! Thank you.
Dr. William Martin: I do believe in the stability “dip” between primary (at placement) and secondary (at osseointegration) time points, this is the focus point in the manufacturing of the “perfect” implant, creating an implant design and surface that eliminates the “dip”. I just didn’t mention it in my lecture due to topic and timing of my presentation.
If the reading is 50 after 3-months – will you load?
Dr. William Martin: What was it at placement? Did it decrease? What does the radiograph look like? Where is it located in the mouth? Was there grafting done and what was the timing of placement? These are all questions I would have to determine whether I would load or not. But, after 3-months, I agree that it is time to do something.
What is the best grafting material?
Dr. William Martin: Sorry, I cannot answer this question. Site and indication specific, there is not one graft material for all situations.
How or where can I learn about digital implant workflow?
Dr. William Martin: Reach out the implant company you work with and inquire on course offerings, or you can visit www.iti.org and explore the ITI Online Academy, there is plenty of content there to view. In addition, becoming a member of the ITI will give you access to publications (ITI Treatment Guides) that focus on that specific topic.
On multiple implants every reading, are you using the same peg for ISQ reading?
Dr. William Martin: At the time of surgery, we will use the same SmartPeg for multiple implants, but if/when we get readings that don’t correlate with our clinical findings, we will utilize a new SmartPeg. In my experience, they are often good for a few implants prior to replacing. But remember, this is at the same visit and time, we do not sterilize or use them at later dates.
What ISQ measurements are indicated for different implant loading strategies?
Dr. William Martin: Please see below.
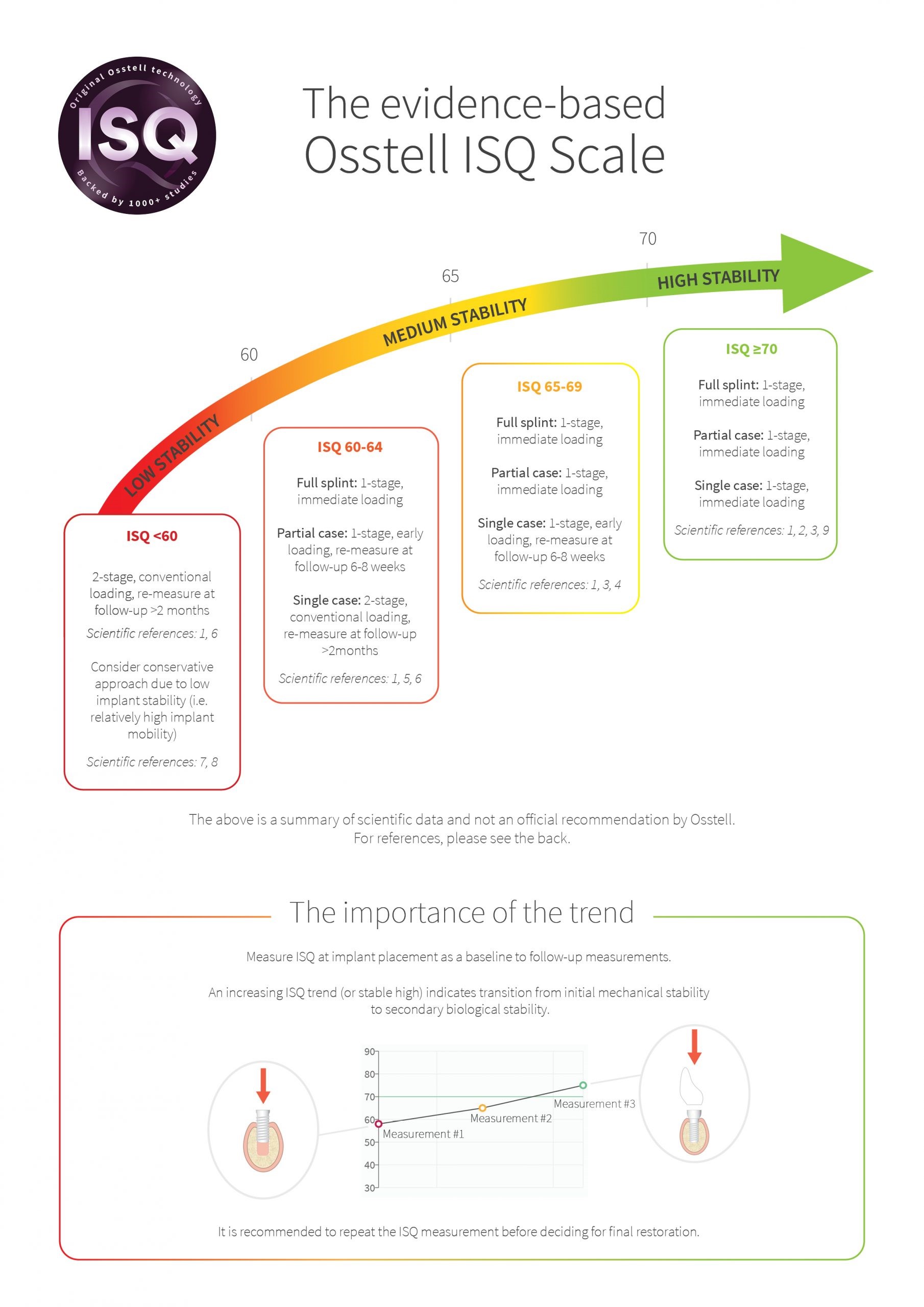
So if ISQ is <60 during full arch case for a single implant, which loading protocol would you suggest and what is the significance of ISQ measurements in such cases?
Dr. William Martin: We have situations where at the time of placement of a single implant the ISQ is 60 or less. We will follow a conventional loading protocol, 8-12 weeks healing – evaluate ISQ, if improved then load. If the ISQ is the same, we will load. If the ISQ decreases, we will utilize other clinical factors to determine course of action – 1) longer healing or 2) remove.
The ISQ measurement is working in conjunction with other clinical evaluations, it is not the sole determinator for treatment direction. We need to use clinical expertise and knowledge when at all possible.
Thank you everyone joining us at the Osstell Scientific Symposium. See you again next year!
You can watch the webinar on-demand here.
More information about the symposium can be found on www.osstellcampus.com.


Add comment