Proven in Everyday Practice
Oct 16, 2015
Prof. Daniel Buser (University of Bern, Switzerland) on Implant Stability and the Implant Stability Quotient (ISQ)
If you ask patients about their expectations of an implant treatment, the answer is almost always to get results as fast as possible – in addition to a largely pain-free treatment and the desire for aesthetically pleasing results. The desire to meet these expectations without compromising predictability, reliability and sustainability of the final prosthesis, has resulted in an increasing challenge for surgeons and dentists.
Under these circumstances, measuring implant stability is an essential diagnostic tool. Since the earliest developments in 1999, Osstell has continuously worked to develop a technology that measures the stability of the implants objectively and non-invasively by using resonance frequency analysis (RFA) and the Implant Stability Quotient (ISQ), in order to help dentists meet the demand for reduced implant treatment times, while still avoiding premature loading. Marianne Steinbeck, project manager of BDIZ EDI, spoke with Prof. Daniel Buser (Bern, Switzerland), who took part in the development as one of the scientific advisers.

Where do you see the main benefits of measuring implant stability?
In the past 15 years, we have been able to significantly shorten the healing times for implant patients. While immediate loading is mainly used for edentulous patients, we are today able to apply early loading in approximately 80 percent of the cases with partially edentulous patients with inter-dental space, free-end edentulism or single-tooth gaps. This means healing periods of four to eight weeks. If you work in a team, the dentist has to decide when an implant can be loaded. To minimize the risk of loading the implant too early – which is linked to the risk of having the implant fail – you have to measure the implant stability in an objective way. The best way to do that is currently with ISQ measurements. After initial challenges the technology has now matured and is well documented by countless clinical studies.
Is insertion torque not a sufficient indicator of how stable the implant is? What about the good old tap test?
Insertion torque can be used to measure primary stability, but follow-up measurements are not possible. This means you don’t have a way to measure secondary stability during the healing period to assess the bone apposition at the implant surface.
That’s the biggest weakness of insertion torque measurements. The good old tap test is entirely antiquated and does not meet today’s requirements in any way.
What advantages do ISQ values have?
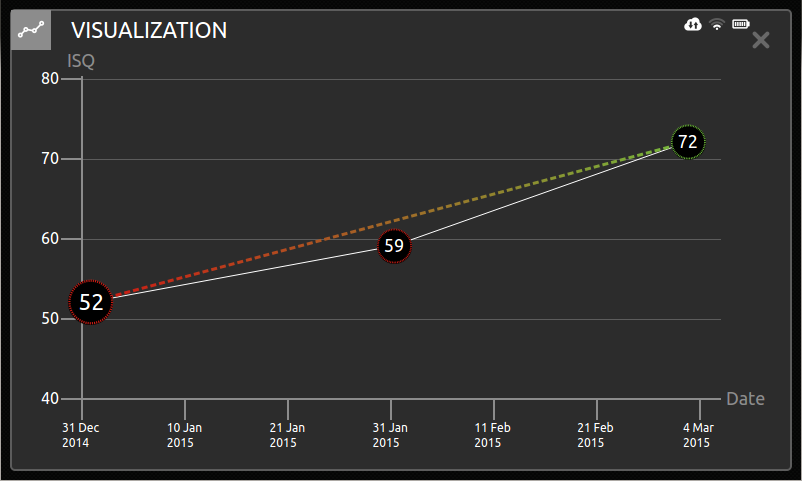
Clinical experience over the last 10 years show a high reliability for the ISQ measurements that are done in the mesio-distal directon . It means that we measure right after placing the implant to have the baseline value. Depending on planned healing time, the measurement is repeated after four or eight weeks. If the ISQ value is ≥ 70, the implant will be released for final restoration. If the ISQ value is below 70, the healing time will be extended by four more weeks. This process has been well proven in the daily practice.
Do patients understand this additional treatment?
The required time is minimal, but the communication with patients much easier because the measured value can be visualized. With a high-tech device patients feel safer and that’s why the acceptance is very good.
Thank you, Prof Buser, for your time and this conversation.
This interview was originally published in BDIZ EDI (3/15)