By Francisco Teixeira Barbosa
Every day we do a lot of things based on our intuition. We make decisions based on our own or others experience.
We do not need science to help us in our daily life, and we don’t have a clear indicator that shows us if our decision is the best.
Decisions based on practical experience is our way of life.
But when it comes to our profession as dentists, we do, or at least we should, evidence-based dentistry for…almost every treatment we perform.
As the title of this article says, I´m going to present a case about “progressive loading.”
Yes, I know, progressive loading is supported by few clinical studies (Rotter 1996, Appleton 2005, Ghoveizi 2013), but -and here comes the interesting part- the rationale behind this concept makes sense from a clinical and biological point of view.

Let me explain it.
Some implants at the end of the osseointegration period have less than 25% of the overall surface in contact with the surrounding bone (Misch 1993).
Although they have a low BIC values, they are clinically stable. However, this stability may be lost in the medium or long term when the implant is loaded with the definitive restoration.
Problems are more likely to occur if the bone density around the implant is low and as we all know, poorest bone density is present in the posterior maxilla (Norton 2001) although there can be different bone density in various regions of the jaw (Parker 2008, Fuh 2010).
How to improve bone density around implants during the healing period?
At the moment no method exists that is clinically validated and predictable to augment bone density around an implant. (Click to Tweet)
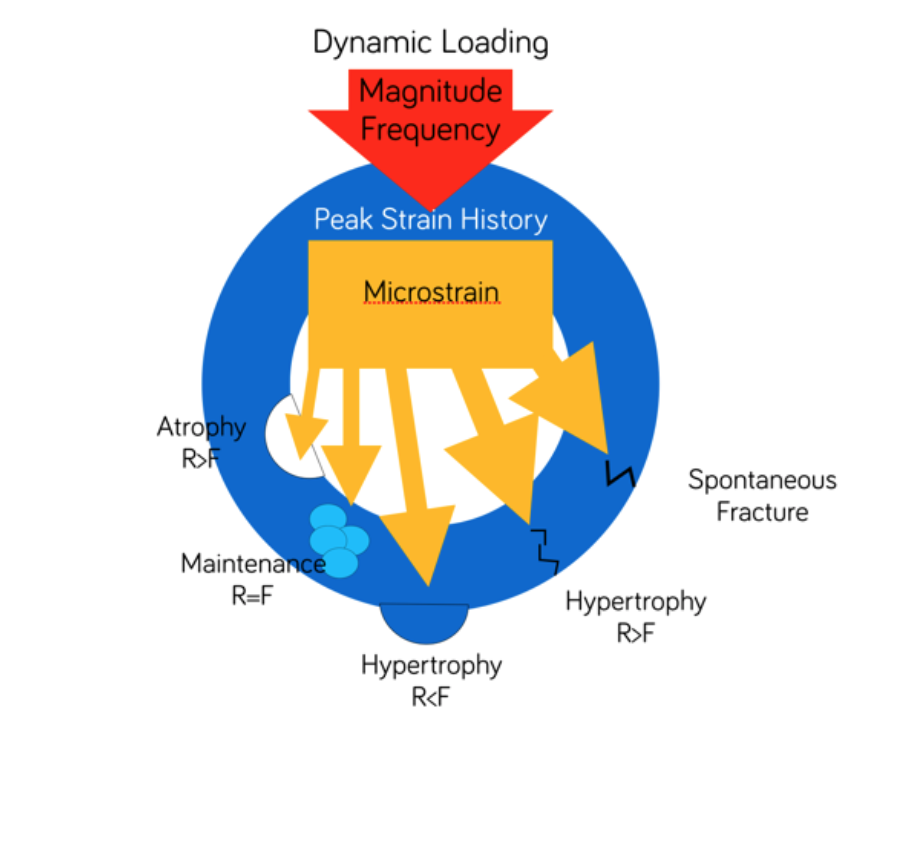
Regarding Frost´s “mechanostat theory,” the enhancement of bone density is a result of a dynamic relationship between loading and positive bone modeling response (Frost 1983, Frost 1987).
|
At this point, we can start introducing the concept of progressive loading:
Applying forces gradually to the implant will allow a positive bone modeling response, increased peri-implant bone density which will allow the whole complex bone-implant-restoration to withstand occlusal load.
This is important mainly in the posterior maxilla where the bone quality is lower and biological complications are more likely to occur (Nevins 1993).
Clinical case:
A patient with a horizontal fracture of a canine. Good general health conditions, non-smoker.
 |
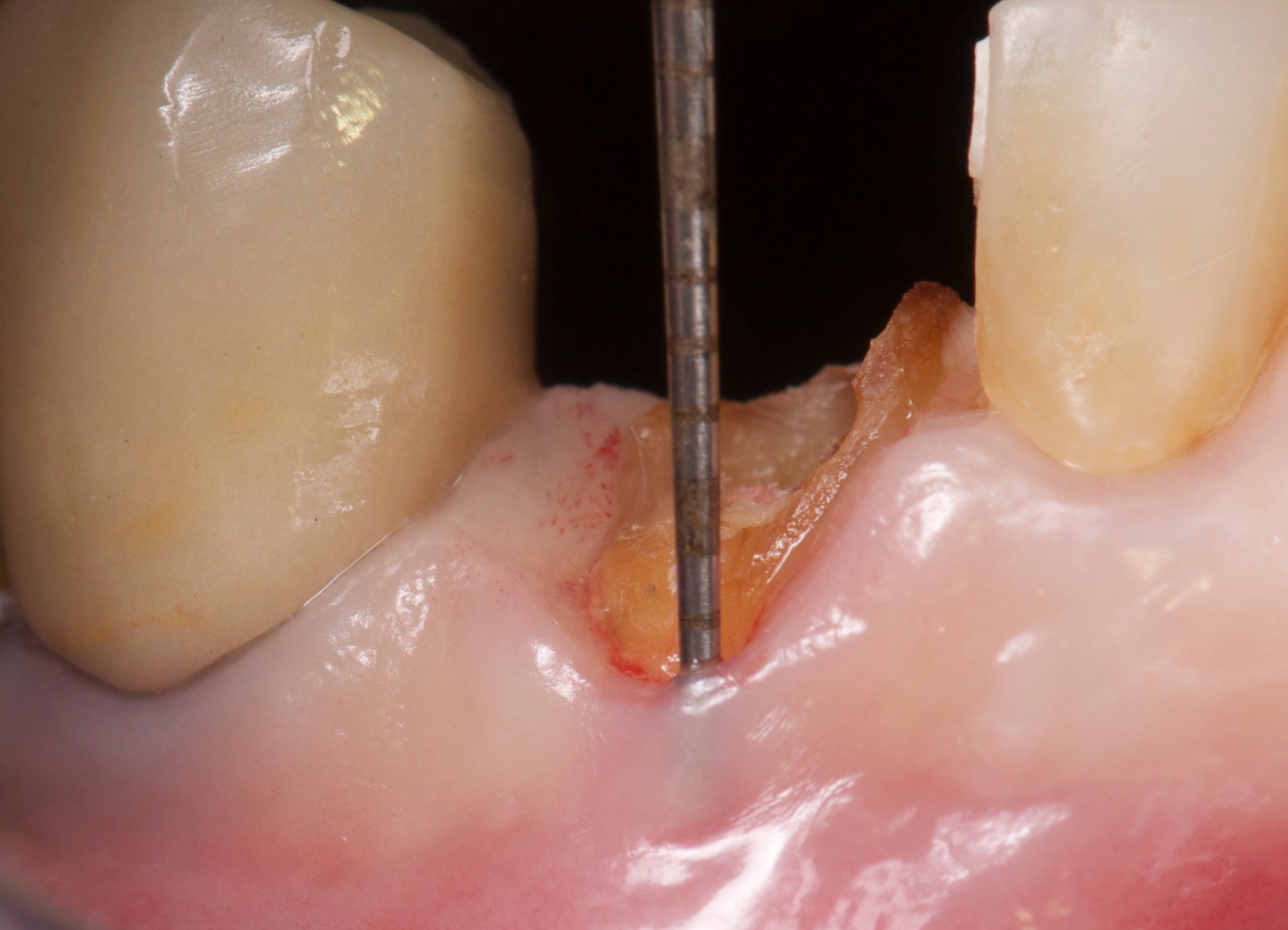 |
After evaluation of the tooth remnant, we decided to carry out a ridge preservation with Bio-Oss® and close the socket with a combination epithelized-subepithelial connective tissue graft (Stimmelmayr 2010).
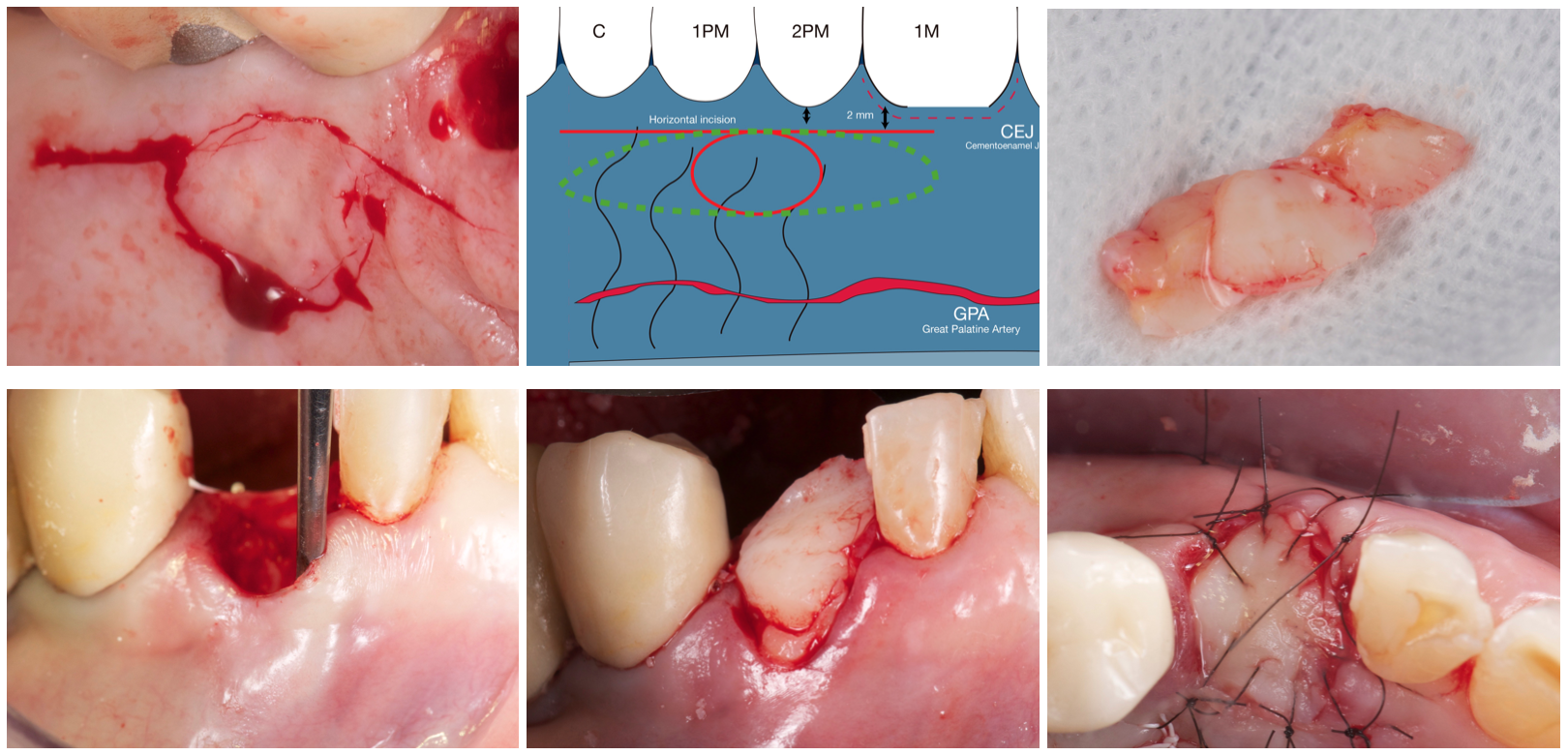
This combined technique has advantages over the free gingival graft (Landsberg 1994, Jung 2004):
- Reliable primary wound closure was provided after ridge preservation or immediate implant placement.
- The papillae of the neighboring teeth were supported.
- Displacement of the mucogingival junction was prevented.
- The labial and crestal soft tissue were thickened.
- Survival of the onlay component of the graft was ensured.
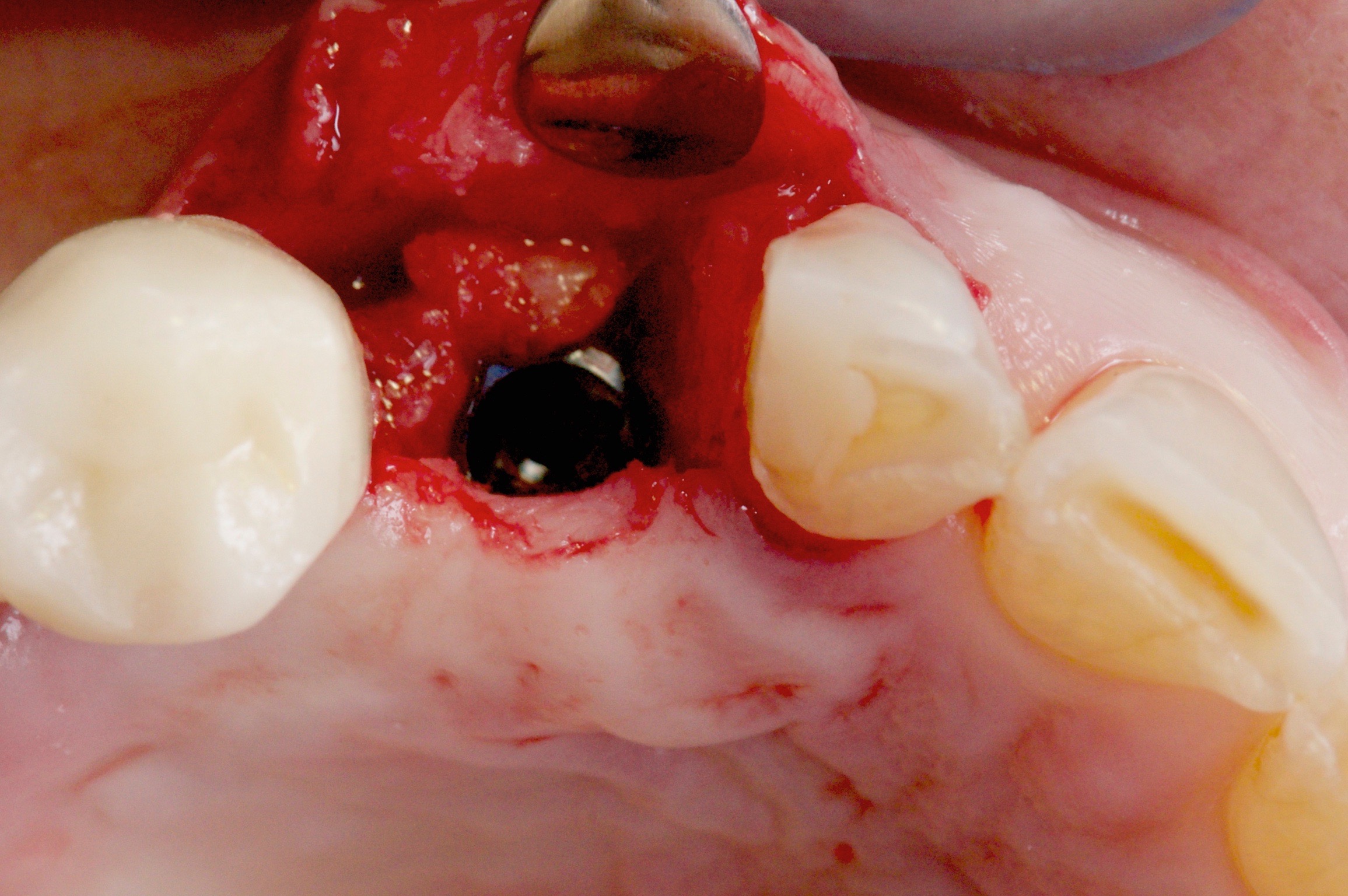
After waiting four months, we placed the implant (Phibo Aurea 4,3×13 mm).
Lately, we are waiting no more than four months after a ridge preservation (De Risi 2013):
- There are no histological advantages in waiting more time. More information in this infographic.
- We can engage the implant apically and meanwhile the osseointegration process is paired with the graft maturing process.
After placing the implant, the ISQ value was 77 which is a high value even though it was placed in a grafted site (Zita 2017).
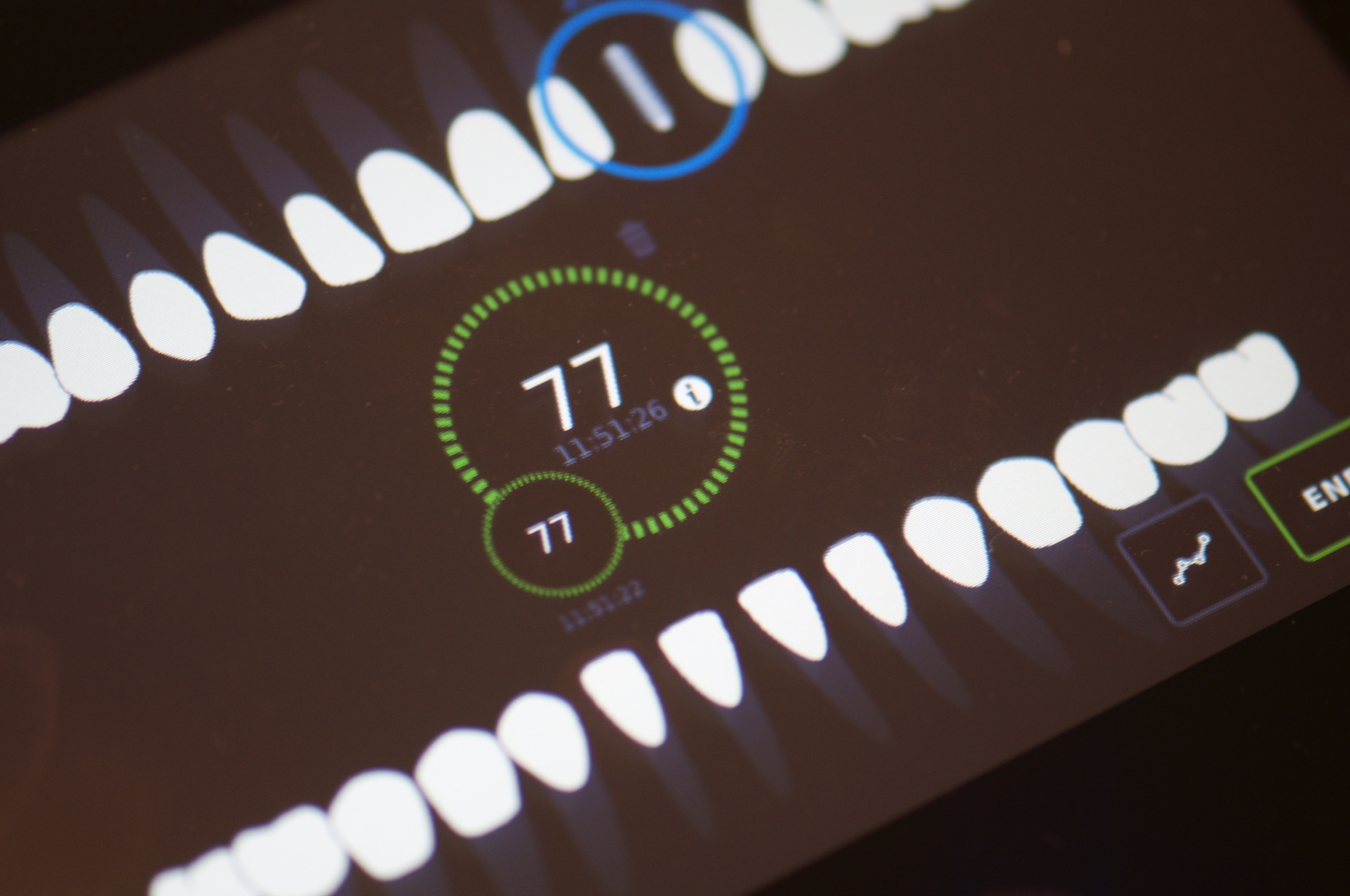
After one month and a half, we did the second surgery, and again the ISQ was measured.
This time something unexpected was happening: The ISQ value had dropped almost 20 points, which is a sign that something is wrong.
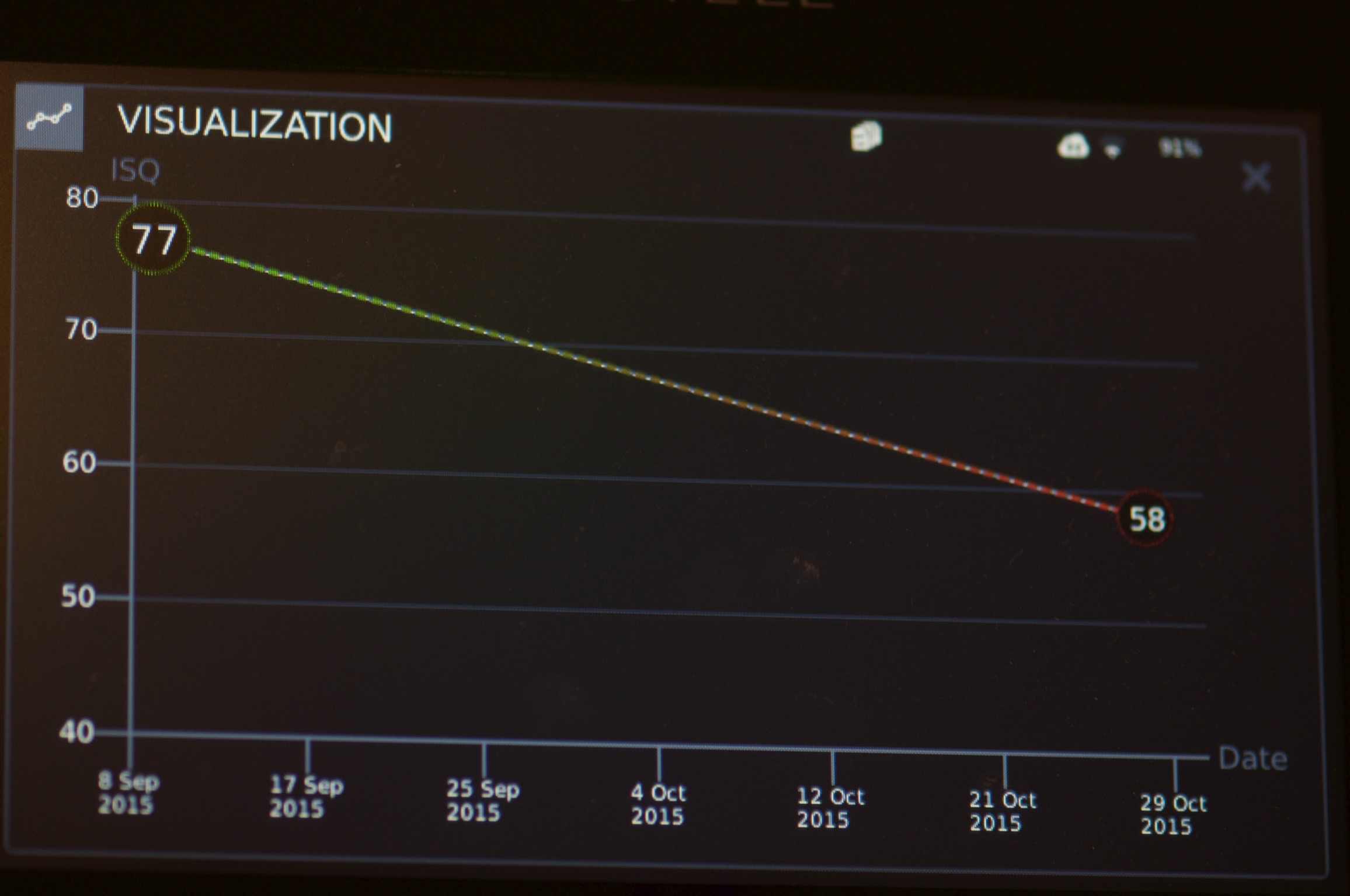
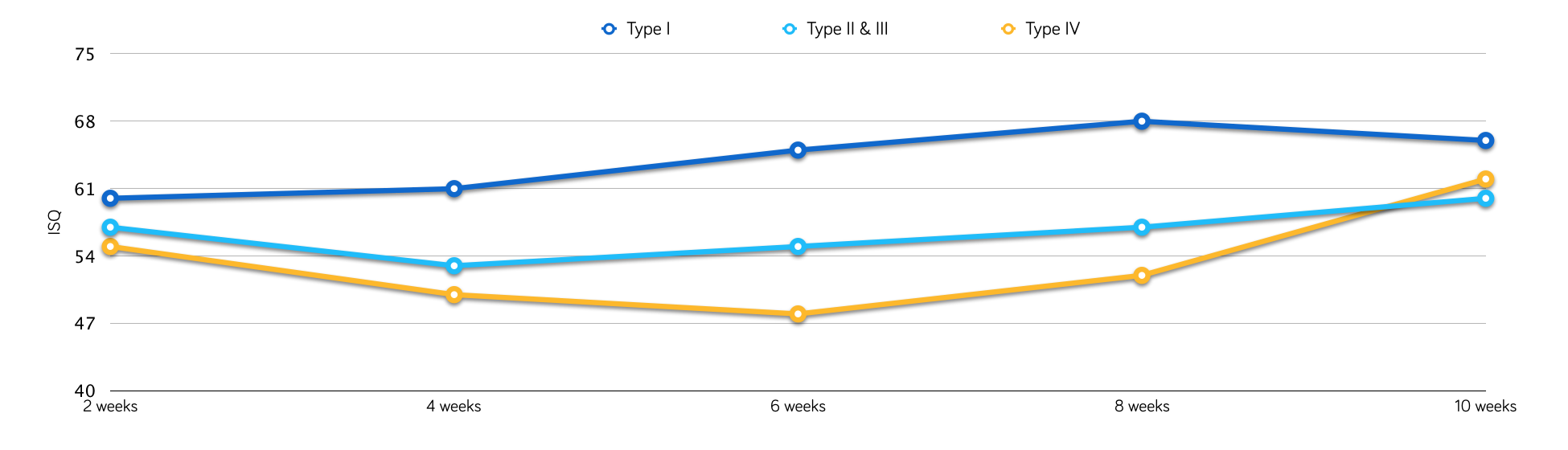
There is always a variation in the ISQ during the osseointegration process, and values usually go down initially (first few weeks after implant placement), depending on the quality of the bone where the implant was placed (Barewall 2003).
Two decisions are possible here:
- Remove the implant
- Try a progressive loading in attempt to increase the ISQ value (from stimulating the bone remodeling).
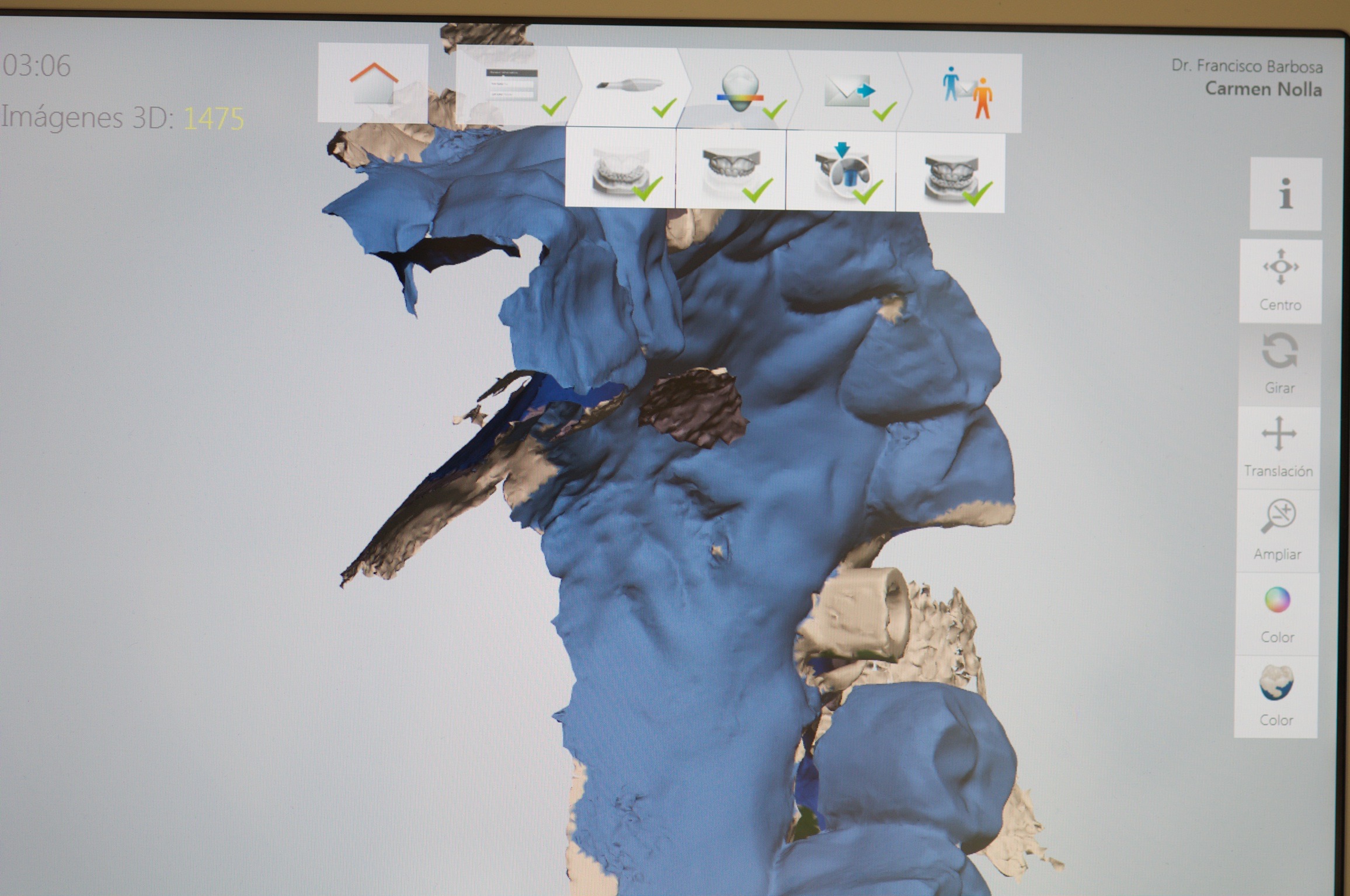
We decided to perform a digital impression with the 3Shape Trios 3 and order two PMMA provisional restorations designed and manufactured in CAD/CAM (Phibo CAD/CAM. Barcelona. Spain).
Why two provisionals?
1) First, we designed a provisional restoration out of occlusion with the antagonist to observe if there was any ISQ value progression over time.
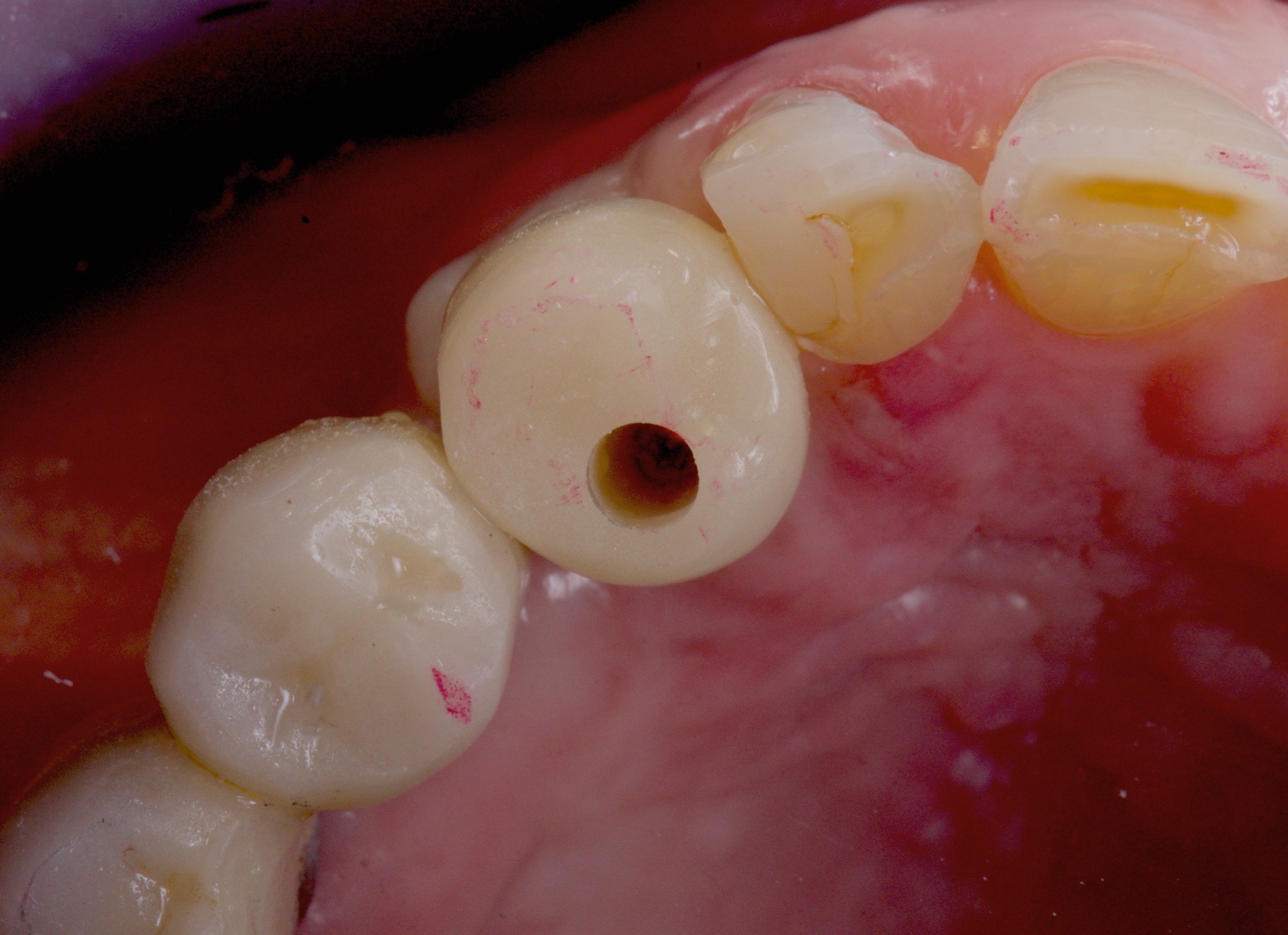
2) If there was any improvement in the ISQ value, the initial provisional was then substituted with a functional provisional.

After one month, the ISQ value was up almost 10 points, and we decided to deliver the second provisional with functional contact.
Three months after the second provisional was delivered, the ISQ value was already up to 70 ISQ, and we decided to perform the definitive restoration.
It is not a beautiful outcome, but the patient accepted the definitive aesthetic result and the restoration were screw-retained with a torque of 35 NCm.

Conclusions
Although the limitations of this short case report, we conclude that using ISQ measurements (RFA) to monitor bone remodeling before delivering a definitive restoration can improve the survival rate of the global rehabilitation.
The uncertainty of the BIC (bone implant contact) between the implant and the bone and also the resistance of the implant to the micromovement at the time of the definitive loading, justifies the use of the ISQ measurement to monitor the implant behavior during osseointegration.
It was also proved that the Osstell® ISQ might also indicate information about the bone density around an implant, which can be of great value in the posterior maxilla (Manresa 2013).
Of course, a lot of questions are left to answer yet, like:
- If the ISQ value has no relation with the BIC (Abrahamsson 2009), why is it still of great value to make clinical decisions in cases where we are not sure to load the fixture?
- If the ISQ has a no direct relation with the BIC, why do values improve overtime when we perform a progressive loading?
- Should ISQ be mandatory in cases where patients have non-optimal general health conditions (diabetes, osteoporosis) or smokers?
- Should provisionalization be mandatory in cases after a guided bone regeneration?
Hope you enjoyed the article and I would love to hear your feedback.

Add comment