Background: Scott D. Ganz, DMD
Could you please introduce yourself to our readers and tell us a little bit about your background?
Dr. Scott Ganz: I started my dental education at the University of Medicine and Dentistry – now known as Rutgers School of Dental Medicine, and followed that with a three-year specialty program in Maxillofacial Prosthetics at M.D. Anderson Cancer Center in Houston, Texas. I have been involved with both the surgical and prosthetic phases of dental implants since 1982, and started my involvement with the use of CT scan technology since 1985. My career has focused on the use of 3-D imaging modalities for diagnostic, surgical, and treatment planning applications in dentistry, including the evolution of CAD CAM digital workflows and have published extensively on these topics, including contributing to more than a dozen textbooks. I have also been fortunate to have served as a consultant to the dental industry in different technical areas for more than 28 years, and as an international educator / speaker at various venues around the globe. I currently serve as Editor-n-Chief for Cone Beam International Magazine of Cone Beam Dentistry, and Assistant Editor for the peer-reviewed journal, Implant Dentistry among other publications. I maintain a private practice in Fort Lee, New Jersey.
How do you use Osstell in your clinic?
Dr. Scott Ganz: Placing dental implants is serious business, and I feel that it is important for clinicians to know how to diagnose and treatment plan with the most useful tools. In my clinical practice of implant placement and restoration, the most important tools are CBCT imaging modalities for proper diagnosis of potential implant receptor sites, and the IDx Osstell resonance frequency analysis to determine implant stability. Essential for ALL cases performed in my office.
What are the main benefits you see from using Osstell? What advantages do ISQ values give you?
Dr. Scott Ganz: The benefits of having an objective manner in which to assess implant stability cannot be underestimated. The key word here is OBJECTIVE… as resonance frequency analysis (RFA) measures the frequency of vibration by means of a sensor called a SmartPeg, connected to an implant helping to record a “stiffness” value. This value or “Implant Stability Quotient” (ISQ) can then be recorded as part of the patient chart, and provides invaluable information to the clinician in terms of the stability of the implant – apart from the amount of frictional torque necessary to deliver the implant to the osteotomy site at that moment in time. The second advantage is that the ISQ values can be measured over TIME, which is extremely important when monitoring when to load an implant, when to restore, or to determine if an implant may be failing.
What type of surgical protocol are you using today? How do you decide which protocol to use?
Dr. Scott Ganz: First, as a surgical prosthodontist, my goal is always to understand that patients are not coming to me to have implants, they are coming to me to replace missing TEETH. The new digital workflows make it easier to determine implant receptor sites based on restoratively-driven planning utilizing CBCT and the 3-D assessment of individual anatomical presentations. Often we need to replace all of the structures that are missing including bone and soft tissue, and therefore ancillary bone or soft tissue grafting maybe required. My decision making process is based upon accumulating as much diagnostic information as possible to take the guesswork out of the equation.
Has the loading protocol been decided before you place the implant, or does that change depending on your assessment?
Dr. Scott Ganz: As each patient presentation and anatomy is individual and different, the first assessment of the pre-existing condition is made with the use of 3-D imaging and treatment planning software. Understanding the density of the bone, thickness of the cortical plates, trajectory of the bone, opposing occlusion, etc. helps to decide the protocol used for implant placement. This could be conventional two-staged approach where the implant is buried under the soft tissue, a one-staged approach where a healing collar may be attached to the implant and left exposed in the oral environment, or an immediate loading / immediate restoration protocol. Therefore based on 3-D planning, many decisions are possible in advance of the surgery – however it is not until the implant is actually placed into the bone that the clinicians is truly aware of its stability. It is at that moment where it is essential to know the ISQ value to finalize the most acceptable treatment protocol.
So in your experience, what kind of ISQ value are you targeting?
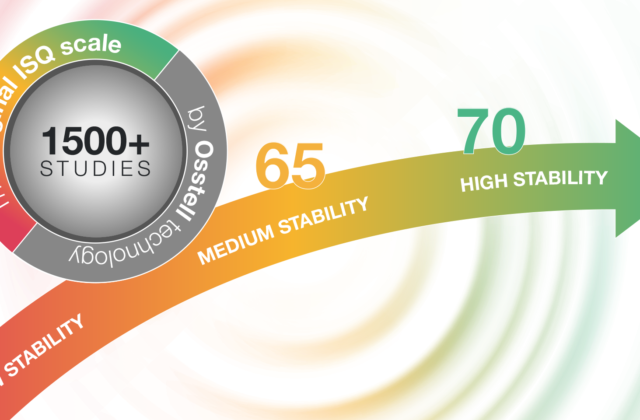
Dr. Scott Ganz: Osstell is fortunate to have over 800 articles in the literature to help provide clinicians with the confidence to apply the ISQ scale of values to their patient. That stated, there has to be a full understanding of the clinical presentation and desired occlusion or restorative result. A single implant between two natural teeth is a different presentation than a single implant in the most distal placement in posterior mandible against natural opposing teeth. The single implant in a protected environment may be loaded with a lower ISQ value than a stand-alone implant in the posterior mandible or maxilla. Accordingly the same applies when multiple implants are being placed, i.e. splinting vs non-splinting to gain cross platform stabilization.
Clinical experience therefore needs to be exercised to appreciate how best to use the ISQ scale on a case-by-case basis. Generally though, I like to see ISQ values above 70 as an indicator for loading.
Do you communicate around the ISQ value with the patients? Do you explain it to them?
Dr. Scott Ganz: As with many diagnostic tools, I feel that it is very important to explain to the patient why it is essential for the planning process. Therefore I review all of the CBCT scans with the patient to go over their individual clinical presentations, the quality and quantity of bone, and where we need to place implants or bone grafting. The same applies to ISQ values… in fact I often like to make predictions with my staff and the patient once an implant is placed… and we read out the values to give the patients additional confidence about the treatment that they are receiving. This can be viewed as a positive marketing strategy – but more importantly it becomes part of the medical-legal information in the patient chart where the status of the implant(s) can be monitored over time.
Before using Osstell, how did you assess implant stability?
Dr. Scott Ganz: The same way that most clinicians do – we looked at the torque values at implant placement.
What are your thoughts on using insertion torque or tapping when measuring implant stability? Are they sufficient indicators?
Dr. Scott Ganz: The drilling protocol is usually determined by the implant manufacturer which can affect the insertion toque based on the size and shape of the osteotomy, the dimensions of the implant (most importantly diameter), and design of the threads. Insertion torque can be measured continuously when the implant is rotated into the osteotomy site as it corresponds to the friction between the implant and the walls of the osteotomy which could be straight or tapered. So insertion torque can vary, and often is a totally subjective measure of the bone-to-implant friction at that moment in time. Therefore it can give the clinician a false sense of confidence that the implant is stabile. Tapping on an implant may provide an audible sense of confidence – but cannot discriminate or provide a necessary value that confirms whether an implant is sufficiently integrated for loading.
How much does a failure cost? What will the patient say?
Dr. Scott Ganz: No one want to have an implant fail. That stated, implants can and do fail. Patients need to be aware of the risks of the procedure. Many times we just are not certain why an implant fails – however if an ISQ value is recorded on placement, upon loading, and monitored over time, we can at least establish a baseline for success, or if poor values are noted, we can make a decision to remove the implant before it gets to the restorative phase where additional costs are involved with the dental laboratory. Failures are costly in both the monetary sense and the time required for the multiple office visits, and potential loss of confidence by the patient.
What do you think will change in implant dentistry over the next 5 years?
Dr. Scott Ganz: Generally the world of dental implants will continue to evolve and improve with innovative designs, surface technology, materials that are utilized, as well as the techniques used for various treatment modalities. Technology will continue to provide new and exciting tools for the surgical aspect as well as the restorative phases of implant dentistry… hard and soft tissue grafting applications will also continue to be a major focus of our industry as will the influence of rapid prototyping or 3-D printing as part of the changing digital workflows.
What trends are you seeing in the industry?
Dr. Scott Ganz: The use of CBCT continues to be widely accepted as an important diagnostic modality, with more and more emphasis on combining the digital workflows of the dental laboratory, intra-oral optical scanning, desktop scanning, and 3-D printing applications. CAD CAM technology has also continued to develop and innovate.
Who inspires/d you the most in your career? How/Why?
Dr. Scott Ganz: As my area of interest is mainly dental implants, imaging applications, and digital technologies, I have been inspired by all of the dental implant pioneers who helped pave the way for what we do today. Clinicians who take the time to document and publish, who spend countless hours on research, or putting together presentations that inspire or motivate others to adopt, change, or get involved in our field of interest. There are too many to name here – although it’s appropriate to mention two giants that we recently lost, Dr. Leonard Linkow, and Dr. Carl Misch. Enough said that I appreciate all of their often monumental efforts which continue to inspire me today.
Dr. Scott Ganz will be holding a Hands-on workshop at AO 2017, Orlando:
“Assessing Implant Sites for Delayed and Immediate Protocols: CBCT and RFA/ISQ as Critical Diagnostic Tools”
Why did you chose these themes/cases for the workshop?
Dr. Scott Ganz: I believe that clinicians can learn from a variety of different didactic clinical case presentations – however often the hands-on portion is on generic models, or animal jawbones. With today’s technology is it possible to take the CBCT dataset, and export the shape of the mandible or maxilla from an actual case that has been documented through the use of 3-D printing. Hopefully this will facilitate a more meaningful hands-on exercise for the participants. They will get to practice on mandibles that were real cases, and perhaps they will understand how to apply the concepts described in the workshop to their own patients based upon this experience.
What do you recommend Dentists about to start placing implants? What kind of educations/training do you recommend?
Dr. Scott Ganz: Unfortunately, I believe that even today, most dentists do not get a lot of clinical experience placing or restoring dental implants while in dental school, or even in many post-graduate programs. Therefore, clinicians must seek out other educational opportunities to expand their knowledge base. Organizations like the Academy of Osseointegration help to provide these opportunities – and what is especially useful are the hands-on workshops which offer a smaller, more intimate setting for direct learning. I am also fortunate to be involved in many educational offerings and I feel that after a hands-on workshop that live surgery courses offer an important bridge for learning to enhance a clinician’s ability to treat their own patients. More information can be found at www.handsonsurgery.org or www.aiedental.com