Meet Drs. McClain & Schallhorn
Feb 1, 2016
Speakers at the Corporate Forum at AO 2016
Could you please introduce yourself to our readers and tell us a little bit about your background?
My name is Pamela McClain. I’m a Periodontist and have been practicing for 28 years. I am a past President of American Academy of Periodontology and a diplomate of the American Board of Periodontology. We have been very fortunate to participate in clinical research in our practice including several FDA trials. I’ve also had the opportunity to provide continuing education through lecturing at various venues in the US and abroad. I’m thrilled that I’ve been able to practice with my father, Dr. Robert G. Schallhorn, for 20 years, and now with my niece, Rachel Schallhorn.
My name is Rachel Schallhorn. I’m a private practice Periodontist. I’ve been in private practice for about 6.5 years. I did my specialty training at the University of Texas, San Antonio. I’ve been involved in clinical research, published several articles related to periodontal disease, and also done some lecturing. I’m also a past President of The Rocky Mountain Society of Periodontists.
How do you use Osstell in your clinic?
Dr. McClain – We use it to get a baseline measurement at the time of implant placement on all of our implant cases. It helps us decide if the case is a good case for early loading, or whether we need to bury the implant. Most implants we do are one stage, or single stage.
Dr. Schallhorn – We use it to determine when we’re ready to restore the implant. To me it’s an objective tool to really assess our implant stability. On most cases, we take a second reading around three months post-surgical. If I don’t feel the implant is ready at that time, I will recheck every four to six weeks after that.
What are the main benefits you see from using Osstell? What advantages do ISQ values give you?
Dr. McClain – It’s an objective tool to determine implant stability and it’s a way we can track stability over time. It’s an additional piece of information for the decision making during surgery. The biggest advantage is to have an objective measurement tool in cases where the bone quality is less than optimal.
What type of surgical protocol are you using today? How do you decide which protocol to use?
Dr. Schallhorn – The majority of our implants are single stage. Occasionally I will do a 2 stage procedure if the stability isn’t good and if I have a low ISQ value. I don’t do immediate or early loading very often. However, if we are going to do early or immediate loading, the ISQ is very important.
Dr. McClain – It’s basically the same for me; I do primarily single stage. I will do two stage more often in the maxilla or with sinus elevation cases or where the ISQ is below 60.
Has the loading protocol been decided before you place the implant, or does that change depending on your assessment?
Dr. Schallhorn – For me, it can change. The protocol is not set in stone before the implant is placed and I get the ISQ value. I’ve actually started checking patients at six weeks if there was a high initial ISQ, in order to give restorative clearance a bit sooner. Whereas in the past we had them wait at least three months. So I usually wait until I get that [ISQ] measurement to really know how to proceed.
Dr. McClain – I agree with Rachel. I came from the old Brånemark days, where you waited six months for everyone. So to load the implant in three months is a big step for me. One of the biggest advantages with using ISQ values is to allow earlier loading and final restorations for patients.
“One of the biggest advantages with using ISQ values is to allow earlier loading and final restorations for patients.”
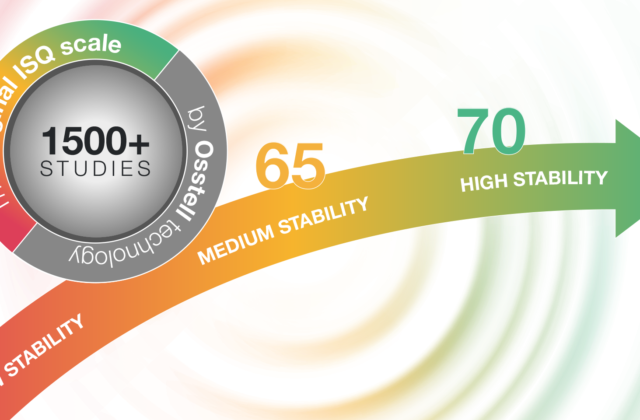
So in your experience, what kind of ISQ value are you targeting?
Dr. Schallhorn – 70 or above.
Dr. McClain – I agree. Depending on the implant size a minimum measurement of 60 is necessary but if the value is over 70 I feel much more confident about the implant stability.
Do you communicate around the ISQ value with the patients? Do you explain it to them?
Dr. McClain – Yes, and we also communicate the value with the restorative dentist. We’ve been doing this for over 6 years and have found it to be a good objective tool to inform our colleagues about when the patient is ready for the restorative phase.
Before using Osstell, how did you assess implant stability?
Dr. Schallhorn – It was subjective. Basically torque value on placement and then tactile feel, which is not a very good measurement.
Dr. McClain – Like Rachel said, it was very subjective. You relied on torque value, radiographs and gut feeling.
What are your thoughts on using insertion torque or tapping when measuring implant stability? Are they sufficient indicators?
Dr. McClain – Insertion torque has been used for many years to determine implant stability at the time of placement but the ISQ values are more objective.
Dr. Schallhorn – There is something to be said about the experience of placing 100s of implants, and getting a feel for how stable the implant will be. Everyone gains wisdom with experience. ISQ increases the chance for success and helps us guide the treatment of the patient.
How much does a failure cost? What will the patient say?
Dr. Schallhorn – You need to consider the monetary cost, but also how that impacts the patient’s confidence in you. I would say a failure is pretty costly in many respects.
Dr. McClain – The cost to replace a failed implant is more costly than placing the initial implant. It’s financially more costly, because of the additional time it requires to manage the case. It’s also the patient’s time and more importantly the potential disappointment with the surgeon.
What do you think will change in implant dentistry over the next 5 years? What trends are you seeing in the industry?
Dr. Schallhorn – I see a trend moving towards shorter treatment times and quicker loading protocols. I would say, once a week people ask me about “teeth in a day”. So everyone wants it fast and they want it now. If there’s a viable option for shortening treatment times, we would certainly consider it to get our patients their end results quicker. But we want to be pretty sure that it is going to work, by good indicators of stability, before we commit to a shorter protocol. The decision about shortening the treatment time is based on initial implant stability and bone quality. The patient’s systemic health is also a major factor.
Who inspires/d you the most in your career? How/Why?
Dr. McClain – My father, Dr. Robert Schallhorn, who was a pioneer in Periodontics with his innovative bone grafting techniques and the research he did that really changed how we practice Periodontics today. He has been a wonderful mentor and teacher for me in my career.
Dr. Schallhorn – I’d second that, but I would say Pam as well. Not just as a Periodontist, but also as a person.
Don’t miss Drs. McClain and Schallhorn’s lecture at the Osstell Corporate Forum at the
Annual Meeting of the Academy of Osseointegration in San Diego, CA