Over the years, there have been many developments in the field of implant dentistry that help to improve clinical outcomes, such as new implant surfaces, innovations in implant design and components, and advanced grafting products and techniques for site development. We now see success and survival rates that consistently exceed 95% and are attributable to these state-of-the-art implant technologies, clinical expertise, case selection and patient compliance.
Historically, when root-form implants were first placed, they were submerged during osseointegration. Later, non-submerged implants with delayed loading became the typical protocol and shortened treatment times. Today, patients want well-functioning, natural-looking restorations and prostheses as soon as possible following surgery. As a result, patients are increasingly demanding shorter treatment times and patients who historically would not have been candidates for implant treatment due to compromised bone and other risk factors are requesting implants. Therein lays the dilemma, as for some patients their clinical condition (for example, porosity of the recipient bone bed, limited bone volume or medical conditions) lengthens the bone reparative process which requires longer healing periods. This makes it crucial to be able to objectively measure primary implant stability and osseointegration.
The majority of my implant cases are now early loading cases. A minority are immediate loading, and delayed loading is now only performed when immediate or early loading are not advisable. The Osstell technology provides me with an invaluable objective measurement of primary implant stability and the progression of osseointegration over time. That helps me to decide the time of optimum loading.
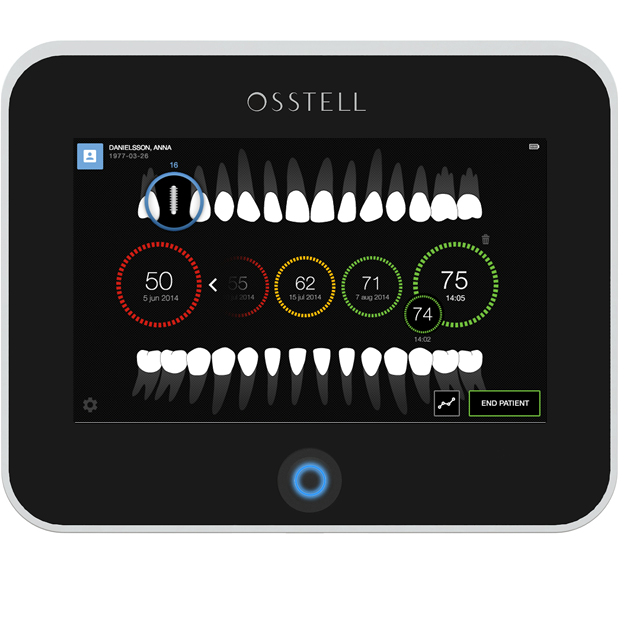
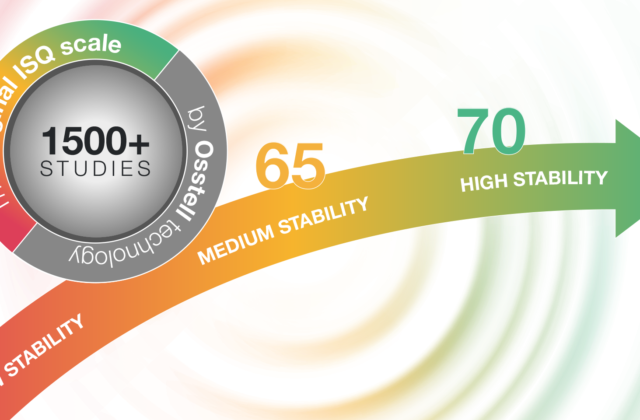
At this point, we have routinely used the Osstell ISQ for over 10 years to identify implant stability and to monitor osseointegration. By providing an objective and reproducible guide for my decisions concerning loading protocols, this technology has helped my restorative referrals avoid potential lost revenue due to implant failures associated with improper healing periods, and to optimize the clinical outcome of implant treatment for patients. Osstell ISQ is reliable and clinically proven, with more than 700 articles published supporting the underlying technology and the use of implant stability quotient (ISQ) measurements to assess implant stability and osseointegration.
 Basically, the Osstell instrument uses magnetic resonance to measure implant stability and the degree of osseointegration at implant sites. Unlike the traditional method of assessing implant stability and osseointegration by measuring torque, which could be hard to objectively quantify and could on occasion negatively influence stability, the Osstell ISQ method is completely noninvasive and objective.
Basically, the Osstell instrument uses magnetic resonance to measure implant stability and the degree of osseointegration at implant sites. Unlike the traditional method of assessing implant stability and osseointegration by measuring torque, which could be hard to objectively quantify and could on occasion negatively influence stability, the Osstell ISQ method is completely noninvasive and objective.
Using this method, a small, high-precision metal rod (the SmartPeg) is attached by screwing it into the internal thread of the implant or the implant abutment complex. Next, the Osstell probe is placed in close proximity to the SmartPeg and emits magnetic pulses that cause the SmartPeg to resonate. The resonance varies depending on the lateral stability of the implant and the rigidity of osseointegration, and is interpreted using resonance frequency analysis (RFA).
Therefore, a comparison can be made between the readings obtained immediately following implant placement (baseline) and those obtained at a given moment during osseointegration. In this way, the degree of osseointegration can be determined. In addition, any observed decreases in ISQ from one time point to another can indicate potential problems and enable early intervention. Showing the readings to patients also helps involve them in their treatment. I have found that most patients appreciate this information and understand the decision on when to load their implants. Readings above 55 ISQ have been validated to indicate an acceptable degree of implant stability for loading.
Osstell ISQ helps prevent failures and the associated costs for the office and patients. Overall, the main advantages for my office and patients are the quality assurance we have been able to implement into implant protocols, the ability to reduce treatment time through earlier loading, and the ability to manage implant risk. Osstell has become my personal guide in determining the appropriate time to load patients’ implants, and I now use it for every implant case.